Case Report - Ophthalmology Case Reports (2018) Volume 10, Issue 1
Achromatic choroidal melanoma: Case report and literature review.
Yonli Yempabou Hugues Arnaud*
Department of Ophthalmology, Chouaib Doukkali University, El Jadida, Morocco
- Corresponding Author:
- Yonli Yempabou Hugues Arnaud
Department of Ophthalmology,
Chouaib Doukkali University,
El Jadida,
Morocco
E-mail: arnaudhugues10@gmail.com
Received: 20-Apr-2023, Manuscript No. OER-23-96590; Editor assigned: 24-Apr-2023, OER-23-96590 (PQ); Reviewed: 09-May-2023, QC No. OER-23-96590; Revised: 23-Jun-2023, Manuscript No. OER-23-96590 (R); Published: 30-Jun-2023, DOI:10.35841/oer.7.5.171
Citation: Arnaud YYH. Achromatic choroidal melanoma: Case report and literature review. Ophthalmol Case Rep. 2023;7(5):1-2.
Abstract
Objective: To describe a case of achromatic melanoma.
Result: This is a retrospective case of a 39 years old female patient with a visual acuity decrease of 06/20 OD, in whom the biomicroscopic examination was normal, with a fundus in favour of a nonpigmented mass with retinal detachment at OD. B-mode ultrasound revealed a hyperechoic domed mass. The characteristic T1 hypersignal and T2 hyposignal appearance and enhancement after injection of gadolinium was found on MRI and management was enucleation of the right eye. The diagnosis of choroidal melanoma was confirmed on pathological examination, which found a spindle cell type.
Keywords
Achromatic melanoma, Biomicroscopic, Retinal detachment, Hyposignal appearance, Spindle cell
Introduction
Choroidal melanoma is a primary malignant tumour secondary to the anarchic multiplication of choroidal melanocytes. It is a rare disease with an estimated incidence of 500-600 new cases in France, which most often affects people over 50 years of age. Choroidal melanomas can be pigmented or achromic. The latter type is the least frequently found. We report a case of achromatic melanoma in a 39 years old female patient.
Case Presentation
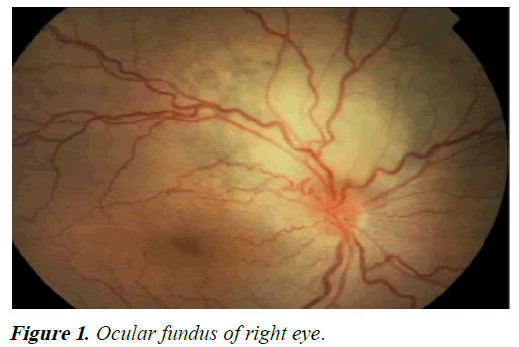
The patient was 39 years old and had no previous history of melanoma. She was consulted for a decrease in visual acuity of 06/20 OD and 18/20 OG. The examination with the optical biomicroscope was without any particularities in both eyes. The ocular fundus and fluorescein angiography revealed a suspicious mass in the upper temporal region of the right eye opposite a retinal pallor associated with retinal detachment and venous tortuosity. Examination of the left eye was normal (Figures 1 and 2).
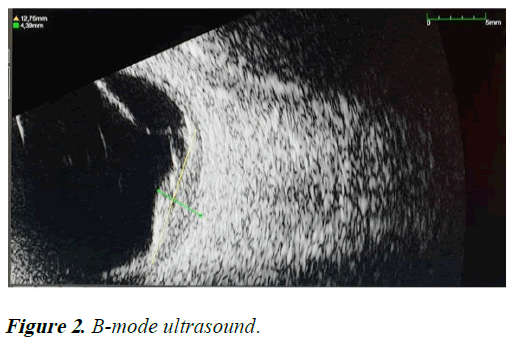
B-mode ultrasound revealed a dome shaped hyperechoic choroidal mass with retinal detachment in the right eye. The imaging was completed by an orbitocerebral MRI which revealed a suspicious mass in hyposignal T1 and hypersignal T2, with gadolinium uptake, suggesting in the first instance to be correlated with anatomopathological data. The patient’s extension work-up was negative.
Management consisted of enucleation of the right eye after informed consent under general anaesthesia.
Histological examination of the excisional specimen found a brownish lesion measuring 12 mm × 10 mm+tumour proliferation of essentially spindle shaped architecture with anisokaryotic and strongly nucleated nuclei in favour of a choroidal melanoma (Figure 3).
Discussion
Choroidal melanoma is a primary malignant tumour located in the posterior uvea and represents the majority of intraocular cancers. It is a rare disease in general but has a poor prognosis because of the risk of metastasis, that is why early diagnosis is important [1,2].
The most frequently found clinical sign is a decrease in visual acuity [3]. On the fundus, melanoma can have several aspects: Pigmented or achromatic. The particularity of achromatic melanoma is that it can go unnoticed on the fundus, thus delaying diagnosis and management. It should be noted that a normal fundus does not rule out the diagnosis of ocular melanoma [4]. B-mode ultrasonography can reveal suggestive images: A hyperechoic mushroom or dome shaped mass frequently associated with retinal detachment [5]. Fluorescein angiography shows a double circulation in the early stages and pinpoints in the late stages. On indocyanine green angiography, the choroidal circulation is well visualised. This allows the differential diagnosis between malignant and benign lesions [6]. Orbito cerebral MRI in favour of melanoma is a suspicious mass in T1 hypersignal and T2 hyposignal and enhancement after injection of gadolinium with restriction.
Management, after the extension assessment, is currently varied, ranging from mutilating surgery: Enucleation; to conservative techniques: Proton therapy, brachytherapy, thermotherapy [7-9]. The confirmatory diagnostic examination is pathological anatomy. The prognosis is mainly related to the metastatic risk which depends on the size of the tumour, the age of the patient and the underlying chromosomal abnormalities.
Conclusion
Achromatic choroidal melanomas are rare but serious tumours that require careful ophthalmologic examination to avoid being missed. An early diagnosis would allow a better management with the arrival of new therapies particularly effective for small tumors.
References
- Shields CL, Manalac J, Das C. Choroidal melanoma: Clinical features, classification and top 10 pseudomelanomas. Curr Opin Ophthalmol. 2014;25(3):177-85.
[Crossref] [Google Scholar] [PubMed]
- Oksala A. Echogram in melanoma of the choroid. Br J Ophthalmol. 1959;43(7):408-14.
[Crossref] [Google Scholar] [PubMed]
- Apt L. Uveal melanomas in children and adolescents. Int Ophthalmol Clin. 1962;2(2):403-10.
- Su GW, Yen MT. Current trends in managing the anophthalmic socket after primary enucleation and evisceration. Ophthalmic Plast Reconstr Surg. 2004;20(4):274-80.
[Crossref] [Google Scholar] [PubMed]
- Desjardins L, Levy C, D’Hermies F, et al. Initial results of proton therapy in choroidal melanoma at the d’Orsey center for proton therapy; the first 464 cases. Cancer Radiother 1997;1(3):222-6.
[Crossref] [Google Scholar] [PubMed]
- Nag S, Quivey JM, Earle JD, et al. The American brachytherapy society recommendations for brachytherapy of uveal melanomas. Int J Radiat Oncol Biol Phys. 2003;56(2):544-55.
[Crossref] [Google Scholar] [PubMed]
- Oosterhuis JA, Journee-de-Korver JG, Kakebeeke-Kemme HM, et al. Transpupillary thermotherapy in choroidal melanomas. Arch Ophthalmol. 1995;113(3):315-21.
[Crossref] [Google Scholar] [PubMed]
- Shields CL, Kaliki S, Furuta M, et al. Clinical spectrum and life prognosis of patients with uveal melanoma based on age at presentation in 8033 cases. Retina. 2012;32(7):1363-72.
[Crossref] [Google Scholar] [PubMed]
- Parrella P, Sidransky D, Merbs SL. Allelotype of posterior uveal melanoma: Implications for a bifurcated tumor progression pathway. Cancer Res. 1999;59(13):3032-7.
[Google Scholar] [PubMed]