Research Article - Biomedical Research (2017) Volume 28, Issue 3
A study on the performance of sounds control program on some physiological parameters of premature infants hospitalized at infants special care units (NICUs) of selected hospitals of Shiraz University of Medical Sciences in 2013
Marzie Kargar1*, Fatemeh Hashemi1, Bahare Beh Amooz1, Seyed Mostajab Razavi2, Seyed Mohamad Javad Mortazavi3 and Najaf Zare41Collage of Nursery and Obstetrics, Shiraz University of Medical Sciences, Shiraz, Iran
2Infants Medicine fellowship (PHD), Shiraz University of Medical Sciences, Shiraz, Iran
3Medical Physics PHD, Shiraz University of Medical Sciences, Shiraz, Iran
4Biostatistics PHD, Shiraz University of Medical Sciences, Shiraz, Iran
- *Corresponding Author:
- Marzie Kargar
Collage of Nursery and Obstetrics
Shiraz University of Medical Sciences, Iran
Accepted date: May 23, 2016
Abstract
Background: The purpose of this study is to investigate the effect of sounds control program on some physiological parameters of premature infants and on sounds intensity level of NICUs.
Methods: 20 premature infants at fetal age of 30-34 weeks and weight of 1000-2000 g were selected randomly. Before the intervention, blood oxygen saturation percentage, heart rate, respiration rate and their fluctuations were measured and recoded as well as the sounds intensity level at the infants care unit 3times a day (morning, afternoon and night) for one week. The intervention program was performed along the next week and all measurements were done at one, two and three weeks after the intervention. Data were analyzed by SPSS software after collection and multi sample repetitive scales variance test, post huck banferoni test and paired T test were performed.
Results: Sounds intensity average and its maximum and minimum, before the intervention at three shifts showed that they are all more than standard (45-50 db). There were no significant differences detected in blood O2 saturation percentage, and heart rate and their changes before and after the intervention but respiration rate and its changes were significantly decreased (p-value<0.05). By recognizing and control of sounds resources the total mean sounds intensity and total mean of maximum sounds intensity were decreased by 7.79 db and 13.07 db, respectively.
Conclusion: Sounds intensity at NICUs is more than standard level and this can have a relation with increased mortality of premature infants therefore it must be controlled and decreased.
Keywords
Sound, Infant, Premature, Physiological parameters.
Introduction
The fetus can receive many sounds in the uterus. It records his/her mother's sounds and this is very effective on his/her speaking pattern development in future. The amniotic fluids protect the fetus against loud and sever sounds harms but after birth the infant is purely defenseless. Sounds intensity is much higher when passing through air than amniotic fluids and its harms on infant's auditory system and other physiologic parameters and his/her development is more adversely effective [1]. Anatomic and self-regulatory systems are weak in premature infants therefore they are more vulnerable to loud and sever sounds and this is related to their inability in filtering and decreasing the harmful stimulants [2]. The Auditory system is so much developed even in premature infants at 26-28 weeks that this loud sound can cause physiological alterations in their heart rate, blood pressure, respiration rate and O2 saturation percentage and therefore maintaining a stable physiological condition is very hard for them [1]. Regarding to Nagorski, sounds pollution can adversely affect the stability of infant's physiological signs, auditory system, neurological development, sleeping rhythm and [1] Infants hospitalized at NICUs are exposed to sounds louder than standard that can adversely affect their health especially their cardiovascular and respiratory systems even during a short period of time [2].
Slevin et al. [3], Johnson et al. [4] and Zahr et al. [5] expressed that sounds pollution at NICUs causes decreased O2 saturation (and increased oxygen demand, O2 therapy, respiratory care and support requirement), blood pressure increase or decrease (that these incidental blood pressure fluctuations can increase the chance of cerebral hemorrhage in the infant), increased heart rate and respiration rate and sleep disorder. They all mean prolonged hospitalization period, increased treatment expenses and other hospitalization caused problems and infections that can cause many devastating and long term adverse effects in the future of the neonate [6]. Brandon et al. showed that exposure to sounds of 80 db and louder in premature infants can cause apnea, bradycardia, heart rate fluctuations, intracranial hypertension, hyperglycemia, hypercholesterolemia, muscular hyper tension, auditory disturbances and disorders, immunity malfunctions, sleeping disturbances, behavioral disorders (crying and restlessness) and blood pressure, O2 saturation and tissue blood perfusion level fluctuations [7]. In a study performed on 34-35 weeks premature infants, it was revealed that sudden sounds can increase restlessness, crying, hypoxia, intracranial pressure, apnea and respiration rate. These all can decrease brain blood flow [2].
Other studies showed that adverse effects of loud sounds in NICUs can cause cardiovascular system stimulation, auditory decrease and weakness, increased gastric secretion, adrenal and hypophysial stimulation, immune response suppress against infection and female infertility [8]. Sounds intensity recommended by International Noise Council is 45 db during morning work shift, 40 db during afternoon and 20 db during night with the range of ± 3 db [9]. Sounds intensity level control in NICUs is one of the most important goals of AAP and suggests that sounds level at infants surrounding environment must be lower than 45 db and louder temporary sounds must not be higher than 65 db. It is proved that 20 db increase higher than the standard is equal to 10 times increase in the amount and intensity of sounds. 6 db increase will double the sounds intensity [10]. WHO expresses that sounds level increase during the night more than 30 db, will lead to neonatal sleeping disturbance, it is while the intensity of sounds is routinely more than this in hospitals [8].
Through 4 db of sounds intensity decrease, the need to respiratory support and mean diastolic pressure will effectively diminish [11]. Sounds decrease at NICUs is a vital requirement to the infant. Sounds confinement at these units and improving pre mature neonatal growth and health is an indicator of a country development level and it will cause effective costs decrease [12]. Therefore this study was performed in order to investigate the effect of sounds control program at NICUs on some physiological parameters of premature infants and on sounds intensity and level of these units in selected hospitals of Shiraz University of Medical Sciences.
Materials and Methods
This study is a clinical experimental interventional investigation performed on randomly selected 20 premature infants with pregnancy age of 30-34 weeks and weight of 2000-3000 grams without any pathological or organic problems, hospitalized at Hazrete Zeynab and Hafez Hospitals of Shiraz at 1392. At first for one week before and one, two and three weeks after the intervention, the physiological parameters of O2 saturation percentage, heart rate and respiration rate of the infants were measured daily at 3 work shifts of 10-11 morning, 19-20 afternoon and 23-24 night. Oxygen saturation percentages and heart rates were measured by Pulse Oxymeteric device and the respiration rates were measured through abdominal movements count per one minute. Fluctuations of these physiological parameters and the intensity and level of infants unit sounds were measured and recorded by an audiometric device named LT Lutron SL-4013 (made in Finland) once every 10 minutes during other measurements as well.
Hazrate Zeynab Hospital owns 3 NICUs which are placed by each other and each one is connected to the other by a door. NICU1 has 13 active beds, NICU2 has 30 and NICU3 has 11 active beds. Hafez Hospital has only one NICU. Performed sounds control program in these 4 units was as follows:
1. Education to all nursing personnel of NICUs (during a week, 3 one hour sessions, every other day) the classes consisted of booklet presentation, power points, face to face education, interaction with the staff and using their suggestions in order to control the sounds
2. Employing simple strategies to control sounds and sounds pollution alerting devices
3. Supervising strict performance of sounds control program in different working shifts
All recorded data were given to SPSS ver.16 software and were analyzed by multi sample repetitive scales variance test, post huck banferoni test and paired T test.
Inclusion (entrance) criteria
1. Premature infant with pregnancy age of 30-34 weeks and weight of 1000-2000 grams
2. Premature infants must be without any pathological or organic problems such as infections, respiratory distress, cranial hemorrhage,
3. The infant must not be intubated or under the ventilator device
4. Parents willing to participate in the study
Exit criteria
1. Deterioration of infant's general condition or sickness (such as sepsis, cranial hemorrhage, respiratory disorder,)
2. Parents reluctance in participation
3. Infant dismiss or death during study
Results
Sounds intensity before the intervention at morning working shift was 71.84 ± 3.87 db and 69.53 ± 1.37 db for the afternoon and 70.95 ± 5.24 db for the night. Therefore we had the highest sounds level at the morning working shift. One week after the intervention sounds intensity at morning shifts was 66.30 ± 2.83 db and showed 5.54 db decrease. Sounds intensity at 3 weeks after the intervention was 64.78 ± 2.10 db and showed 7.06 db decrease to the week before the intervention. All of these decreases compared to the week before intervention were significant (P<0.05). Sounds intensity before the intervention at afternoon working shift was 69.53 ± 1.37 db and was lower than the morning. One week after the intervention sounds intensity at afternoon shifts was 64.37 ± 3.01 db and showed 5.16 db decrease. Sounds intensity at 2 weeks after the intervention was 63.01 ± 10.64 db and showed 6.52 db decrease to the week before the intervention and at 3 weeks after the intervention was 63.52 ± 2.62 db and showed 6.01 db decrease. All of these decreases compared to the week before intervention were significant (P<0.05).
Sounds intensity before the intervention at night working shift was 70.95 ± 5.24 db and was higher than afternoon and lower than the morning. During one week after the intervention it was 61.37 ± 3.40 db and showed 9.58 db decrease but this decrease was lower than the morning and the afternoon. At 3 weeks after the intervention it was 10.30, the highest amount. All of these decreases compared to the week before intervention were significant (P<0.05) (Table 1).
| Time | Sounds Intensity Average | p-value | |||
|---|---|---|---|---|---|
| One Week before Intervention | One Week after Intervention | Two Weeks after Intervention | Three Weeks after Intervention | ||
| Morning | 71.84 ± 3.87 | 66.3 ± 2.83 | 65 ± 1.3 | 64.78 ± 2.1 | 0.001 |
| Afternoon | 69.53 ± 1.37 | 64.37 ± 3.01 | 63.01 ± 10.64 | 63.52 ± 2.62 | 0.001 |
| Night | 70.95 ± 5.24 | 61.37 ± 3.4 | 64.28 ± 1.95 | 60.65 ± 2.49 | 0.001 |
Table 1. Sounds intensity mean (db) Comparisons before and after the intervention at 3 working shifts.
Respiration rate average per minute before the intervention was 56.50 ± 4.57 at morning, 55.28 ± 5.57 at the afternoon and 56.76 ± 4.54 for the night. Therefore the highest amount was for the night. Till 3 weeks after the intervention it reached to 48.75 ± 2.24 for the morning and showed 7.75 rates decrease averagely. Till 3 weeks after the intervention it reached to 48.13 ± 3.37 for the afternoon and showed 7.15 rates decrease averagely. And till 3 weeks after the intervention it reached to 49.07 ± 4.79 for the night and showed 7.69 rates decrease averagely. Therefore the highest decrease was for the night shift till the third week after the intervention compared with the other shifts. All of these decreases were significant (P-value< 0.05) (Table 2).
| Time | Respiration rates per minute average | p-value | |||
|---|---|---|---|---|---|
| One week before intervention | One week after intervention | Two weeks after intervention | Three weeks after intervention | ||
| Morning | 65.5 ± 4.57 | 51.2 ± 3.57 | 48.24 ± 3.98 | 48.75 ± 2.24 | 0.001 |
| Afternoon | 55.28 ± 5.57 | 51.7 ± 4.62 | 49.55 ± 4.07 | 48.13 ± 3.37 | 0.001 |
| Night | 56.76 ± 4.54 | 53.5 ± 4.56 | 49.63 ± 4.89 | 49.7 ± 4.79 | 0.001 |
Table 2. Respiration rates mean comparisons before and after the intervention at 3 shifts.
Respiration rate fluctuations were also investigated in this study, one week before the intervention at morning shift, the respiration fluctuations mean was 2.65 ± 1.58, it decreased gradually by significant variations at the third week after intervention to 0.62 ± 0.99. It was 2.03 units lower than the pre intervention number. One week before the intervention at afternoon shift, the respiration fluctuations mean was 2.55 ± 1.63, it decreased gradually by the third week after intervention to 0.27 ± 0.71. It was 2.28 units lower than the pre intervention number. One week before the intervention at night shift, the respiration fluctuations mean was 2.69 ± 1.32, it decreased gradually by the third week after intervention to 0.17 ± 0.40. It was 2.03 units lower than the pre intervention number. Therefore 3 weeks after the intervention we had the lowest fluctuations at the night shift and it can be inferred that although respiration rates and respiration fluctuations were also at the normal range before the intervention but they decreased significantly after the intervention (P-value<0.05) and it shows more stability in this parameter after the intervention. This stability is clinically very important to the infant and reflects it's more relaxation in order to reach the optimum growth and development (Table 3).
| Time | Respiration rate fluctuations average | p-value | |||
|---|---|---|---|---|---|
| One Week before Intervention | One Week after Intervention | Two Weeks after Intervention | Three Weeks after Intervention | ||
| Morning | 2.65 ± 1.58 | 0.61 ± 0.69 | 0.4 ± 0.66 | 0.62 ± 0.99 | 0.001 |
| Afternoon | 2.55 ± 1.58 | 0.71 ± 0.96 | 0.5 ± 0.91 | 0.27 ± 0.71 | 0.001 |
| Night | 2.69 ± 1.32 | 1.13 ± 1.08 | 0.3 ± 0.59 | 0.17 ± 0.4 | 0.001 |
Table 3. Respiration rate fluctuations mean comparison before and after the intervention at 3 shifts.
Discussion
This study has been performed on 20 premature infants with pregnancy age of 30-34 weeks (averagely 32 ± 1.11), birth age of 3-5 days (averagely 4.05 ± 0.88) and birth weight of 1000-2000 grams (averagely 1572 ± 279.09). These infants were without any concurrent diseases. In this study, sounds intensity mean till 3 weeks after the intervention at morning shift decreased to 7.06 db, at afternoon shift to 6.52 db, at night shift to 10.30 db and till 3 weeks after the intervention it averagely deceased to 7.79 db. Sounds intensity maximum mean till 3 weeks after the intervention at morning shift decreased to 12.83 db, at afternoon shift to 13.01 db at night shift to 19.5 db, and till 3 weeks after the intervention it averagely and significantly decreased to 13.07 db. These results are compatible with the results of Slevin et al. [3] at Ethics committee of Dublin (hospital). They investigated ''Measuring the effect of silence period protocol at NICUs and its effect on infant's motor responses''. In their study the sound level at normal conditions was 58 db and at silence period decreased to 54 db. Also our results were match with the results study of Elander and Hellstorm [13] in Sweden. They investigated ''the effect of nurses' education on sounds intensity decrease and its effect on infants hospitalized at NICUs'' and could significantly decrease the average sounds intensity level from 57 db to 49 db and control the sound [14].
Also our results are confirmed by the results of Ramesh et al. in India. They investigated '' The effect and expenses of sounds decrease protocol performance on sounds intensity level at NICUs'' and the highest sound level was determined as 60 db. They could decrease it by 2.09 to 9.58 db at different places of NICUs [15]. At the study of Valizade et al. a study on the effect of sounds level decrease intervention on sounds level of Tabriz hospital NICU, The sound intensity decreased by 4 db significantly [16]. Other physiological parameter investigated in this study was the infant's blood oxygen saturation percentage (BOSP). The total average of BOSP at 3 shifts before the intervention was 94.97% ± 1.72% and at one week after the intervention reached to 95.77% ± 1.61% and at 3 weeks after the intervention reached to 95.81% ± 2.03%. Their differences before and after the intervention were not significant.
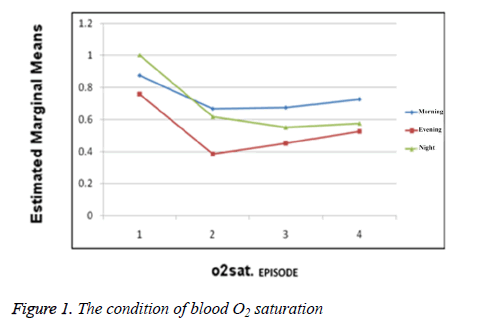
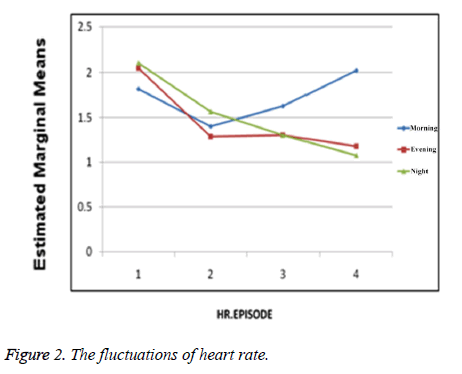
The number of BOSP fluctuations at morning shift was 0.87 ± 0.66. During the first week after the intervention it decreased to 0.66 ± 0.77. At the afternoon shift pre intervention it was 0.75 ± 0.70 and during the first post intervention week decreased to 0.38 ± 0.43. For the night shift pre intervention it was 1.00 ± 0.70 and during the second post intervention week decreased to 0.55 ± 0.87. Therefore these fluctuations have decreased during post intervention weeks; although this decrease is not statistically significant but it shows that the condition of blood O2 saturation percentage is more stable at post intervention weeks and this is clinically very important to premature infants (Figure 1). Other physiologic parameter investigated in this study was infant's heart rate. Heart rates mean before the intervention at 3 shifts was 144.95 ± 10.23 and one week after that reached to 141.84 ± 8.30. Of course this difference was not significant (Figure 2). The heart rate fluctuations before the intervention at morning shift was 1.81 ± 1.13 and one week after that decreased to 1.40 ± 1.11. At afternoon shift pre intervention it was 2.05 ± 1.24 and till 3 weeks after the intervention decreased to 1.17 ± 1.96. Heart rate fluctuations at night shift pre intervention was 2.10 ± 1.50 and till 3 weeks post intervention decreased to 1.07 ± 0.89. Although the fluctuations of heart rate has decreased during the post intervention period but this decrease was not statistically significant, of course it shows that the condition of heart rate is more stable at post intervention weeks and this is clinically very important to premature infants.
Other physiological parameter investigated in this study was the infant's respiration rate. As mentioned before, sounds intensity decrease protocol was significantly effective on this parameter decrease. (P-value<0.05) This result is compatible with the results of Long et al. (1980). Their investigation was performed on 34-35 weeks premature infants and revealed that loud and sudden sounds can cause restlessness, crying, respiratory apnea and respiration rate increase [17]. In order to minimize the harmful effects of sounds pollution during the hospitalization period of premature infants at NICUs, one of important responsibilities of nurses is achieving and obeying the methods of sounds intensity control. Regarding to the results of this study based on positive effects of sounds control program, highest levels of international standards and sounds pollution adverse effects control suggested by AAP can be achieved. We hope that these results might expand the nursing activities field regarding to premature infants care and improve the quality of such cares.
Measurement of sounds intensity at Hospitals of Shiraz University of medical sciences showed that it is much higher than the standard level. Previous studies also had similar results, but in those investigations the sound meter device was placed at one or more certain cites, but in this study the device was portable and was ported by the investigator to places. The advantage of this method is that the sound heard by an individual infant besides the environment background sound (averagely) was calculated and compared by physiological signs of that one infant. A 3 db decrease in environmental sound can make its intensity half. In this study we could decrease the mean sound intensity to 7.79 db and mean total maximum sound intensity to 13.07 db and by this method we reached the AAP standard. Regarding to these results it can be said that sounds control can have positive effects on some physiological parameters such as respiration rate and quality, and our program is more effective because the equipments used in this study can encourage the personnel to consider the principles of sound control program permanently regarding to the education and the booklet that has been presented to them. By continuing investigations and performing more advanced methods in next studies we can hope that sounds adverse effects would decrease and we will have a healthier generation.
In this study blood O2 saturation percentage, heart rate and their fluctuations were also assayed and their differences before and after the intervention were not significant. Possibly it is because of partially stable condition of respiratory and cardiovascular systems of infants. Therefore it is recommended that future investigations would be performed on unstable and ill premature infants at equal conditions. Also the duration of measurements was short in this study (only 3 hours and shifts per day as a sample of 24 hours) and parameter recording consecutively during 24 hours was not possible because of equipments and personnel deficit. Therefore performing such investigations at more equipped centers and with more personnel during 24 hours measurements is recommended. Also such investigations must be performed on more sample populations (in this study 74 infants entered the study but 54 of them exited the study because of dismissing from the hospital and the researcher had to use 2 hospitals) and it is recommended that such investigations be performed on full term or lower than 30 weeks age infants.
Acknowledgment
We appreciate the Researches Chief Assistant of Shiraz University of Medical Sciences because of supervision, confirmation, verification and financial support and also appreciate The Center of Development and Clinical Researches of Namazi Hospital because of statistical support to the research team. This paper has been extracted from the thesis of Bahare Beh Amooz and its financial support is done by Shiraz University of Medical Sciences.
Moral committee certificate code: 92-6850
Clinical experiments recording center code: IRCT2014020116439N1
References
- Joseph A, Ulrich R. Sound control for improved outcomes in healthcare settings. Concord, CA: Center for Health Design 2007.
- Brandon DH, Holditch-Davis D, Belyea M. Preterm infants born at less than 31 weeks' gestation have improved growth in cycled light compared with continuous near darkness. J Pediatr 2002; 140: 192-199.
- Slevin M, Farrington N, Duffy G, Daly L, Murphy JF. Altering the NICU and measuring infants' responses. Acta Paediatr 2000; 89: 577-581.
- Johnson AN. Neonatal response to control of noise inside the incubator. Pediatr Nurs 2001; 27: 600-605.
- Zahr LK, de Traversay J. Premature infant responses to noise reduction by earmuffs: effects on behavioral and physiologic measures. J Perinatol 1995; 15: 448-455.
- Zamberlan-Amorim NE, Fujinaga CI, Hass VJ, Fonseca LM, Fortuna CM, Scochi CG. Impact of a participatory program to reduce noise in a neonatal unit. Rev Lat Am Enfermagem 2012; 20: 109-116.
- Freudenthal A, Van Stuijvenberg M, Van Goudoever J. A quiet NICU for improved infants’ health, development and well-being: a systems approach to reducing noise and auditory alarms. Cognition Technol Work 2013; 15: 329-345.
- Elander G, Hellström G. Reduction of noise levels in intensive care units for infants: evaluation of an intervention program. Heart Lung J Acute Critical Care 1995; 24: 376-379.
- Rabiyan M, Gharib M. Noise pollution in the oprating rooms and intensive care units. Teb va Tazkiye 2003; 51: 50-58.
- Livera MD, Priya B, Ramesh A, Suman Rao PN, Srilakshmi V, Nagapoornima M. Spectral analysis of noise in the neonatal intensive care unit. Indian J Pediatr 2008; 75: 217-222.
- Ranganna R, Bustani P. Reducing noise on the neonatal unit. Infant 2011; 7: 25.
- Nathan LM, Tuomi SK, Müller A. Noise levels in a neonatal intensive care unit in the Cape Metropole. South African J Child Health 2008; 2: 50-54.
- Elander G, Hellstrom G. Reduction of noise levels in intensive care units for infants: evaluation of an intervention program. Heart Lung 1995; 24: 376-379.
- Johnson AN. Adapting the neonatal intensive care environment to decrease noise. J Perinat Neonatal Nurs 2003; 17: 280-288.
- Ramesh A, Denzil SB, Linda R, Josephine PK, Nagapoornima M, Suman Rao PN. Maintaining reduced noise levels in a resource-constrained neonatal intensive care unit by operant conditioning. Indian Pediatr 2013; 50: 279-282.
- Valizadeh S, Bagher Hosseini M, Alavi N, Asadollahi M, Kashefimehr S. Assessment of sound levels in a neonatal intensive care unit in tabriz, iran. J Caring Sci 2013; 2: 19-26.
- Long JG, Lucey JF, Philip AG. Noise and hypoxemia in the intensive care nursery. Pediatrics 1980; 65: 143-145.