Research Article - Journal of Clinical Nephrology and Therapeutics (2022) Volume 6, Issue 2
A study on myocardial performance index in children with nephrotic syndrome in age group 1-12 years.
Tharanidharan SP1*, RK Singh2, Manjusha Goel1, Jyotsna Shrivastava1
1Department of Pediatrics, Gandhi Medical College & Kamla Nehru Hospital, Bhopal, MP, India
2Department of Cardiology, Gandhi Medical College and Hospital, Bhopal, MP, India
- *Corresponding Author:
- Tharanidharan SP
Department of Pediatrics
Gandhi Medical College & Kamla Nehru Hospital Bhopal
MP, India
Phone: +919486377494
Email: dhonidharan@gmail.com
Received: 04-Mar-2022, Manuscript No. AACNT-22-56140; Editor assigned: 07-Mar-2022, PreQC No. AACNT-22-56140(PQ); Reviewed: 14-Mar-2022, QC No AACNT-22-56140; Revised: 18-Mar-2022, Manuscript No. AACNT-22-56140(R); Published: 25-Mar-2022, DOI:10.35841/aacnt-6.2.106
Citation: Tharanidharan SP, Singh RK, Goel M, et al. A study on myocardial performance index in children with nephrotic syndrome in age group 1-12 years. J Clin Nephrol Ther. 2022;6(2):106
Abstract
Background: Nephrotic syndrome (NS) is a common paediatric kidney disease characterised by leakage of protein from the blood into the urine through damaged glomeruli. An increased risk of cardiovascular disease exists in patients with NS because of hyperlipidemia, increased thrombogenesis, and endothelial dysfunction. Objective: Study of Myocardial Performance Index in children with Nephrotic Syndrome and its correlation with age of onset, relapses, hypertension and lipid profile Methods: Total 70 children with nephrotic syndrome of age group 1-12 years included in this observational study. All Children subjected to full history taking, clinical examination and lab studies including serum albumin, serum cholesterol, renal function test. Myocardial performance Index of these children calculated by Doppler Echocardiography using Tissue Doppler Imaging performed in the apical four chamber view. Isovolumetric Contraction time (IVCT), Isovolumic Relaxation time (IVRT), Ejection Time (ET) and MPI were calculated. Results: In our study the mean myocardial performance index is found to be .398±0.045. Significant increase in the Mean Myocardial Performance Index of the patients with the increase in the number of relapse and duration of disease was observed. Myocardial Performance Index has inverse relation with Global ventricular function. Increase in MPI indicate worsening Global Ventricular Function. MPI is significantly higher in patients of Nephrotic Syndrome who had hypertension as compared to patients with normal blood pressure. There is a significant positive correlation between Serum Cholesterol and MPI.
Keywords
Myocardial performance index, Nephrotic syndrome, Hypertension, Hyperlipidemia.
Introduction
Nephrotic syndrome (NS) is a common pediatric renal disorder in India. With an estimated prevalence of 12–16 cases per 100,000 population and annual incidence of~1.5–2 new cases per 100,000 populations, at least 150,000 to 200,000 cases exist amongst Indian children and about 10,000 new cases are added every year [1,2].
Nephrotic syndrome (NS) is the most common chronic renal disease of childhood and the most common type of NS is Primary Nephrotic Syndrome [3]. It is caused by impaired glomerular function, characterized by protein leakage from the blood to the urine through the glomeruli, resulting in proteinuria, hypoalbuminemia, hypercholesterolemia and generalized edema [4]. Apart from hyperlipidemia, a wellknown risk factor for coronary artery disease (CAD) and a defining hallmark of Nephrotic Syndrome, these children also get exposed to other risk factors associated with impaired endothelial function and adverse cardiovascular outcomes like high oxidative stress, frequent infections, sustained proteinuria, hypoalbuminemia and thromboembolism [5].
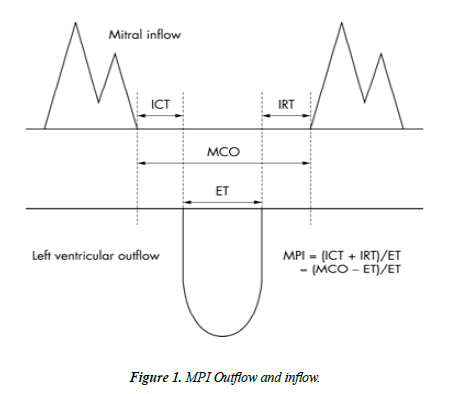
An Echocardiographic/Doppler index of combined Systolic and Diastolic function has been described by Chuwa Tei. Myocardial Performance Index, also called Tei index, is calculated by dividing the sum of IVRT and IVCT by Ejection time (ET). Normally (0.39 ± 0.05). This Tei Index is simple to calculate, reproducible, independent of Heart Rate and Blood Pressure. Measurement of Tei Index is Noninvasive and Easily Obtained, it does not require the presence of an echocardiographer with great experience and it does not materially prolong the time required for examination.
Methods
Children with Nephrotic Syndrome of age group 1-12 years were studied from January 2020 to June 2021 in Department of Pediatrics in a tertiary care Institution. A total of 70 Nephrotic Syndrome Children were enrolled in the study. Sample size was calculated taking the institutional prevalence of admission of Nephrotic Syndrome fulfilling inclusion criteria.
All the consecutively admitted Nephrotic Syndrome Children of age group 1-12 years fulfilling the inclusion criteria of the study were enrolled. Nephrotic Syndrome Children with comorbidities like Congenital Heart Diseases and Severe Anaemia which could independently affect Myocardial Function are excluded. Informed written consent was obtained from parents of eligible Children. Participant’s demographic profile, immunization status, lab parameters were taken and entered into a case record form. Myocardial Performance index assessment was done by the method of Tissue Doppler Echocardiography.
We use Tissue Doppler Imaging performed in the apical four chamber view. Using this method Isovolumetric Contraction time (IVCT), Isovolumeric Relaxation time (IVRT), Ejection Time (ET) calculated. MPI calculated by this formula:
(Isovolumetric Contraction Time+Isovolumetric Relaxation Time)/(Ejection Time)
Taking the reference value of normal Myocardial Performance Index between 0.39+0.05. Blood Pressure, Serum Cholesterol, Serum Albumin of all children were taken. Those Children who were found to have hypertension, hyperlipidemia, and hypoalbuminemia were compared with Myocardial Performance Index (Figure 1).
Data regarding Proteinuria, deranged renal Function tests were recorded and analyzed.
Statistical analysis
The collected data were transformed into variables, coded and entered in Microsoft Excel. Data were analyzed and statistically evaluated using SPSS-PC-25 version.
Quantitative data was expressed in mean ± standard deviation or median with interquartile range and depends on normality distribution. Difference between two comparable groups were tested by student’s t-test (unpaired) or Mann Whitney ‘U’ test while for more than two groups comparison ANNOVA test or Kruskal Wallis H test was used. Qualitative data were expressed in percentage and statistical differences between the proportions were tested by chi square test or Fisher’s exact test. Spearman correlation coefficient was used to correlation between two quantitative parameters. P’ value less than 0.05 was considered statistically significant.
Results
A total of 70 children were enrolled in the study, out of which 59% were males and 41% were females. The mean age of study participants was 5.88 ± 3.13 years with most of the participants belonging to the age group of 6 to 10 years. In our study the mean myocardial performance index was found to be .398 ± 0.045. the MPI increased gradually with relapse and the number of episode in Nephrotic Syndrome and this increase was found to be significant. Mean MPI in patients with 1st episode was 0.365 ± 0.030, in patients with 1st relapse was 0.396 ± 0.048, in 2nd relapse patients were 0.429 ± 0.013 and in frequent relapse cases was 0.450 ± 0.026. Which shows that with increasing frequency of episodes myocardial performance index also increased. (p<0.001) (Table 1).
| No of episodes | N | Mean ± SD | Minimum | Maximum | p value |
|---|---|---|---|---|---|
| 1st episode | 31 | .365 ± 0.030 | 0.32 | 0.45 | <0.001 |
| 1st relapse | 13 | .396 ± 0.048 | 0.33 | 0.46 | |
| 2nd relapse | 15 | .429 ± 0.013 | 0.41 | 0.45 | |
| Frequent relapse | 11 | .450 ± 0.026 | 0.42 | 0.48 |
Table 1: Association of frequency of relapses with MPI.
Myocardial performance Index was significantly higher in hypertensive patients (0.44 ± 0.02) compare to nonhypertensive patients (0.38 ± 0.04) (p value<0.001) (Table 2).
| Hypertension | P value | ||
|---|---|---|---|
| Absent | Present | ||
| Myocardial performance Index | 0.38 ± 0.04 | 0.44 ± 0.02 | <0.001 |
Table 2: Comparison of Myocardial Performance Index between hypertensive and non-hypertensive patients.
There was significant positive correlation between Myocardial Performance Index and total cholesterol level (r value=0.40; p value<0.001) and significant weak negative correlation between Myocardial Performance Index and serum albumin level (r value=-0.30; p value<0.001) (Table 3).
| Myocardial Performance Index | ||
|---|---|---|
| BSA | r value | 0.366 |
| p value | 0.002 | |
| N | 70 | |
| Hb | r value | 0.044 |
| p value | 0.72 | |
| N | 70 | |
| S. urea | r value | 0.085 |
| p value | 0.486 | |
| N | 70 | |
| S. creatinine | r value | 0.226 |
| p value | 0.059 | |
| N | 70 | |
| S. Albumin | r value | -0.305 |
| p value | 0.01 | |
| N | 70 | |
| Total Cholesterol | r value | 0.409 |
| p value | 0 | |
| N | 70 | |
Table 3: Correlation of different parameters with Myocardial performance index.
Discussion
Nephrotic syndrome (NS) is a common paediatric kidney disease characterised by leakage of protein from the blood into the urine through damaged glomeruli. It is classically defined by nephrotic-range proteinuria (≥ 40 mg/m2/hour or urine protein/creatinine ratio ≥ 200 mg/mL or 3+protein on urine dipstick), hypoalbuminaemia (<25 g/L) and oedema [6]. An increased risk of cardiovascular disease exists in patients with NS because of hyperlipidemia, increased thrombogenesis, and endothelial dysfunction [7]. Hypercholesterolemia is strongly associated with severity of hypoalbuminemia, and persistent proteinuria or renal insufficiency also contributes to cardiovascular disease [8].
Present study was an observational study to assess myocardial performance index in children with nephrotic syndrome, during the study, data of 70 children with nephrotic syndrome was collected.
Myocardial performance index is a good indicator of left and right ventricular function and is a prognostic marker of the congestive heart failure [9]. “It is a numeric value, which could be obtained by using cardiac time intervals. This numeric value is defined as the sum of isovolumetric contraction time (ICT) and isovolumetric relaxation time (IRT) divided by ejection time (ET) and could be calculated for each ventricle individually. Myocardial performance index has been invented as a Doppler index of combined systolic and diastolic myocardial performance” [10]. In our study the mean myocardial performance index was found to be 0.398 ± 0.045. Myocardial Performance Index has inverse relation with Global ventricular function. Increase in MPI indicate worsening Global Ventricular Function. In our study MPI increased in children in 2nd relapse, frequent relapses which indicates Myocardial Dysfunction.
The MPI increased gradually with relapse and the number of episode in Nephrotic Syndrome and this increase was found to be significant. There have been no studies in the Indian subcontinent which have explored this relation between relapse and Myocardial Performance Index.
The patient with Hypertension had a significantly higher MPI, the studies in the past have linked the increased MPI with essential hypertension in children [11,12]. Saleh et al, also recorded and increased systolic and diastolic blood pressure in their study subjects.
A significant correlation was established between myocardial performance index and serum cholesterol in our patients, however in the study by Saleh et al an insignificant increased mean cholesterol was found in patients with RV diastolic dysfunction as compared to normal patients, in the study by Caraba et al [1], a strong inverse correlation (r=-0.9399) was also observed between the endothelial dysfunction and total cholesterol in the patients of nephrotic syndrome. Also in the study by Oflaz et al, Coronary flow reserve measurements were negatively correlated with total cholesterol (r=−0.31; p=0.02). However as opposed to our study in which the creatinine was positively associated with MPI there was a negative correlation with endothelial dysfunction with creatinine.
The cardiac performance in the patients of nephrotic syndrome is a sum total of the aetiopathogenesis as evidenced from the present study as well as research done in the past. There is a requirement of regular cardiac monitoring in patients with Nephrotic Syndrome as the risk of progression to cardiovascular disease through accelerated artherosclerogenesis is increased in such patients. There needs to be further exploration of the topic with appropriate randomised controlled trials to quantify the level of MPI in patients of Nephrotic Syndrome as to better use it as a prognostic indicator in such patients.
Conclusion
There was a significant increase in the Mean Myocardial Performance Index of the patients with the increase in the number of relapse and duration of disease. The MPI was significantly higher in patients of Nephrotic Syndrome who had hypertension as compared to patients with normal blood pressure. There is a moderate significant positive correlation between BSA and MPI. There is a significant negative correlation between S. Creatinine and MPI. There is a significant positive correlation between Serum Cholesterol and MPI.
What is already known?
Increase in Serum Cholesterol level and Blood pressure is a prognostic marker for Myocardial dysfunction in children with Nephrotic Syndrome.
What this study adds?
Increasing MPI with Frequency of Relapses reflects deteriorating Myocardial Dysfunction.
Acknowledgement
Nil.
Ethical Clearance
Institutional Ethical Committee, Gandhi medical college, Bhopal; approval Letter Number
537/MC/IEC/2020; dated 04/01/2020.
Funding
No funding sources.
Conflict of Interest
None declared.
Author’s Contribution
Acquisition and interpretation of data, data analysis, drafting the article, and literature review; JS: Concept, interpretation of data and data analysis, drafting the article, and literature review; AA: Data analysis, manuscript review, manuscript editing, revising the article critically for important intellectual content; JS will act as guarantor. All the authors approved the final manuscript.
Disclaimer
None.
References
- Caraba A, Romo?an I. Endothelial dysfunction in the nephrotic syndrome. Med Pregl. 2007;60:66-9.
- Joles JA, Stroes ES, Rabelink TJ. Endothelial function in proteinuric renal disease. Kidney Int. 1999;56:S57-61.
- Nadir SJ, Saleem N, Amin F, et al. Steroid sensitive nephrotic syndrome in paediatrics. Pak J Pharm Sci. 2011;24(2):207-11.
- Skálová S, Podhola M, Vondrák K, et al. Plasmapheresis-induced clinical improvement in a patient with steroid-resistant nephrotic syndrome due to podocin (NPHS2) gene mutation. Acta Medica (Hradec Kralove). 2010;53(3):157-9.
- Tkaczyk M, Czupryniak A, Owczarek D, et al. Markers of endothelial dysfunction in children with idiopathic nephrotic syndrome. Am J Nephrol. 2008;28(2):197-202.
- Cattran DC, Feehally J, Cook HT, et al. Kidney disease: improving global outcomes (KDIGO) glomerulonephritis work group. KDIGO clinical practice guideline for glomerulonephritis. Kidney Int Suppl. 2012;2(2):139-274.
- Lechner BL, Bockenhauer D, Iragorri S, et al. The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Pediatr Nephrol. 2004 Jul;19(7):744-8.
- Zilleruelo G, Hsia SL, Freundlich M, et al. Persistence of serum lipid abnormalities in children with idiopathic nephrotic syndrome. J Pediatr. 1984;104(1):61-4.
- Ärnlöv J, Ingelsson E, Risérus U, et al. Myocardial performance index, a Doppler-derived index of global left ventricular function, predicts congestive heart failure in elderly men. Eur Heart J. 2004;25(24):2220-25.
- Uluçay A, Tatli E. Myocardial performance index/Miyokard performans indeksi. Anadolu Kardiyol Derg. 2008;8(2):143-9.
- Keshri S, Sharma S, Agrawal N, et al. Hypertension and its severity in children with steroid sensitive nephrotic syndrome during remission. Clin Exp Nephrol. 2018 Oct;22(5):1157-62.
- Gupta-Malhotra M, Hamzeh RK, Poffenbarger T, et al. Myocardial performance index in childhood onset essential hypertension and white coat hypertension. Am J Hypertens. 2016 Mar 1;29(3):379-87.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref