Research Article - Current Pediatric Research (2021) Volume 25, Issue 9
A study of the factors causing secondary nocturnal enuresis in children.
Rana Ismail Afram1*, Emtithal A Wahed Muhammad Saeed2, Qutaiba Hatem Mohammed 2
1 Department of Pediatrics, AI-Yarmouk Teaching Hospital, Baghdad, Iraq
2 Department of Pediatrics, Al-Falluja Teaching Hospital, Baghdad, Iraq
- Corresponding Author:
- Rana Ismail Afram
Department of Pediatrics
AI-Yarmouk Teaching Hospital
Baghdad
Iraq
Tel: +964 771-291-3336
E-mail: drnihadkhalawe@gmail.com
Accepted date: 15th September, 2021
Abstract
Nocturnal enuresis is still perceived as a shameful condition and kept as a secret. But there is nothing shameful about bedwetting. Secondary nocturnal enuresis mostly caused by psychosocial factors that may generates psychological problems for the child, especially evident as a deterioration of self-esteem. A descriptive study of secondary nocturnal enuresis to find out what psychological stressful factors that related and lead the child to have secondary nocturnal enuresis. A prospective study included a sample of 45 children with secondary nocturnal enuresis, whom attended to child psychiatric department were evaluated for the age of primary control, age at which the secondary nocturnal enuresis occurred, sex, residence, either urban or rural aria, family history of primary or secondary nocturnal enuresis in parents and sibling, medical illnesses, history of stressful condition, immigration from their houses, death in family, one of the family arrested, birth of a new baby, family problems like divorce, or others emotional or traumatic event, how the family face the problem and how the child feels toward himself. Of the 45 children, the mean age of primary control of day and night urination was 2.5 years the majority of secondary nocturnal enuresis between 5-10 years girls were slightly more affected, most of them from urban aria, no significant history of secondary enuresis in their parents and siblings, thirty eight children (84.4%) had psychological problems before return to secondary nocturnal enuresis from them 14 children (31.1%) had history of traumatic stressful event, eight children (17.8%) had history of immigration from their houses six children (13.3%) had history of death in family. Seven children (15.6%) had medical illnesses that lead to secondary nocturnal enuresis. Eight children (17.8%) have been punished by their family, thirty seven children (82.2%) were enforced and 27 children (60%) had social embarrassment and inferiority feeling. Conclusion: Secondary nocturnal enuresis was predominantly seen in school aged children after stressful traumatic events. Who need psychological support?
Keywords
Secondary, Nocturnal enuresis, Children.
Introduction
Nocturnal enuresis refers to the involuntary passage of urine during sleep in children over the age of five. Enuresis may be primary (estimated 75%-90% of children with Enuresis in which nocturnal urinary control never achieved for at least 6 months) or secondary (estimated 10%-25% of children with enuresis who was dry for at least six consecutive months and then enuresis developed) [1]. Psychologists may use a definition from the American psychiatric association’s DSM-IV, defining nocturnal enuresis as repeated urination into bed or clothes, occurring twice per week for at least 3 consecutive months in a child of at least 5 years of age and not due to either a drug side effect or a medical condition. Even if the case does not meet these criteria, the DSM-IV definition allows psychologists to diagnose nocturnal enuresis if the wetting causes the patient clinically significant distress [2].
Enuresis can occur only at night (nocturnal), which is more common, or only in the day (diurnal) or both [3]. Mon symptomatic enuresis means that there are no day time symptoms to suggest disorder of the lower urinary tract such as overactive bladder. Polysymptomatic or complicated nocturnal enuresis means that the bed-wetting associated with symptoms suggestive of lower urinary tract dysfunction e.g. overactive bladder or organic pathology as daytime incontinence, urgency, frequency, urinary tract infection and chronic constipation [4].
Aim of study
To determine contributing factors that lead to secondary nocturnal enuresis either medical illness or psychological problem and focus on the stressful and anxiety causing events occurring in the lives that need support and counseling for the child and family [5].
Materials and Methods
A prospective study includes 45 children between the ages of (5-15) years. With secondary nocturnal enuresis (children was dry for at least six consecutive months and then enuresis developed). Total of 30 children attended pediatric psychiatry consultation clinic of child's central teaching hospital in Baghdad city and 15 children attended psychiatric consultation clinic of Alyarmouk teaching hospital in Baghdad city during the period between Decembers 1st 2008 to June 30th 2009. Exclusion criteria those with primary nocturnal enuresis [6-10].
Data was obtained by face to face interview with children or their relatives with the help of social worker, including:
•Age of primary control.
•Age at which the secondary nocturnal enuresis occurred.
•Residence, either urban or rural area.
•Family history of primary or secondary nocturnal enuresis in parents and siblings
•Medical illness as UTI, DM, adenoid hypertrophy.
History of stressful condition as
•Delivery of new baby in family.
•One of family in prison.
•Immigration from house.
•Death in family.
•Separation between parents.
•History of any stressful traumatic events.
•Attitude of family if they punish or reinforce the child to pass the problem.
•How the child feels toward himself.
Results
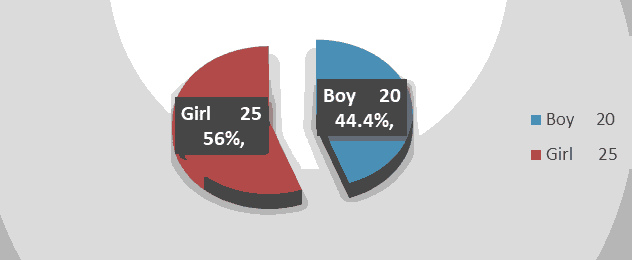
In our sample the mean age of primary control when they control day and night urination was 2.5 years of the 45 children with secondary nocturnal enuresis, the majority of the patients 39 (86.7%) were between age of (5-10) years and 6 (13.3%) between (10-15) years, 20 (44.4%) of them were boys and 25 (55.5%) of them were girls. Boy: Girl ratio=8:10, as shown in the below Table 1 along with Figures 1.
| Age (years) | No. | % |
|---|---|---|
| 5-10 | 39 | 86.7 |
| 10-15< | 6 | 13.3 |
Table 1. Age distribution of cases and their percentage.
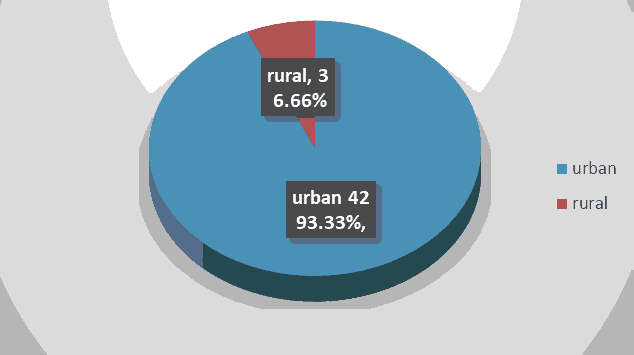
Forty two Children (93.3%) were from urban area while three (6.7%) were from rural area as shown in the Figure 2 below:
Family history for parents and siblings was positive in 6 (13.3%), three of them their father have primary nocturnal enuresis, two of them their mother had primary nocturnal enuresis and one of them his brother has secondary nocturnal enuresis [11-13]. After interviewing the child or his mother with the help of social worker the result has shown that the factors contributed to the secondary nocturnal enuresis are either medical or psychological as shown in the below Tables 2-4.
| Causes | No. | % |
|---|---|---|
| Medical illnesses | 7 | 15.6 |
| Psychological problems | 38 | 84.4 |
Table 2. Distribution of cases according to etiology and their percentage.
| Medical illness | No. | % |
|---|---|---|
| UTI | 4 | 8.9 |
| Adenoid hypertrophy | 2 | 4.4 |
| DM | 1 | 2.2 |
| Total | 7 | 15.5 |
Table 3. Distribution of cases according to medical illness and their percentage.
| Psychological causes | No. | % |
|---|---|---|
| Post traumatic stressful disorders | 14 | 31.1 |
| Immigration from their houses | 8 | 17.8 |
| Death in family | 6 | 13.3 |
| One of the family arrested | 4 | 8.9 |
| Birth of new baby in family | 3 | 6.7 |
| Separation between parents | 3 | 6.7 |
| Total | 38 | 84.50% |
Table 4. Distribution of cases according to medical illness and their percentage.
The above Table shows the medical illness that causes secondary nocturnal enuresis, four children (8.9%) had history of UTI which represents 57.1% of the 7 cases of medical causes; two children (4.4%) had adenoid hypertrophy which represent 28.6% of the 7 cases of medical causes and one child (2.2%) which represent 14.3 of the 7 is newly diagnosed type one DM [14].
The above table show psychological causes related to secondary nocturnal enuresis. Majority of children 14 (31.1%) had enuresis after stressful condition which represent (36.8%) from all children who had psychological stress, eight (17.8%) children had enuresis after immigration from their houses which represent (21.1%) from psychological causes, six (13.3%) children had history of death in family which represent (15.8%) from psychological causes, four (8.9%) children had one member of their family arrested which represent (10.5%) from psychological causes, three (6.7%) children had enuresis after birth of new baby in their family which represent (8%) from psychological causes, three (6.7%) children had enuresis after separation of their parents which represent (8%) from psychological causes. Among 45 children with secondary nocturnal enuresis 8 of them (17.8%) have been punished by their family while 37 (82.2%) children were enforced and reassured by their family to control themselves [15,16]. Of the 45 child with secondary nocturnal enuresis, 27 (60%) had Social embarrassment, anxious, feel different from other and had more inferiority feeling.
Discussion
The mean age of primary control of our sample was 2.5 years and in study done in the United Arab Emirates by Mabrouk for prevalence of nocturnal enuresis most 75% of children attain night time dryness by the age of 3 years. The result in this study show that large no. of secondary nocturnal enuresis were between the age of (5-10 years) which is different from Lane et al. who found that most patients with secondary nocturnal enuresis at age of 4 years and this result difference is because of the effect of traumatic event which are major that happened in our country compared to other problem in others country and no similar study done in countries exposed to similar experiences [17,18]. In study done in the United Arab Emirates for prevalence and correlates of nocturnal enuresis show that 90% of those with enuresis were aged 6-11 years. But in this study primary and secondary enuresis are included. In this study slight significant difference between boy 20 (4.4%) and girls 25 (55.5%). In study done in Jordan for frequency of enuresis in (5-10) year old children, the prevalence of primary and secondary nocturnal enuresis was slightly more frequent in girls than boys [19]. In study done determine the frequency and treatment of enuresis among primary school children living in Oromieh city, Islamic Republic of Iran the frequency of nocturnal enuresis was significantly higher among boys (8.6%) than girls (6.7%) [20].
Another study in north-west Turkey among primary-school children indicated that the rate of nocturnal enuresis prevalence was 8.9% overall, 9.7% in boys and 8.1% in girls [21]. But in these studies primary nocturnal enuresis also included. Most of the children in our study came from urban area 93.3% than the rural area (6.7%) which is higher in comparison with other study done In Saudi Arabia as there was no difference for residency whether rural or urban [22]. This is because the majority of children attended came from area surrounding hospitals which are urban area. In this study, the family history for parents and siblings positive in 6 (13.3%), three of them, were their father had primary enuresis above the age of 10 years, two children their mother had primary nocturnal enuresis and 1 of them his brother has secondary enuresis; While 68.7% have negative history for enuresis. In study done in India for prevalence of primary and secondary enuresis the result was a positive family history for siblings and family members were 28.6% and 19.6% respectively which is higher, this is because the primary enuresis included in their study in which genetics are related more too primary enuresis [23].
In this study causes of the return of bedwetting are either medical illnesses or psychological problem as medical illnesses 7 (15.5%) while psychological problem founded in 38 (84.5%). Of medical illness, in our study 2 children gave history of snoring during night, examination found adenoid hypertrophy. One study reports significant decrease or complete cure of nocturnal enuresis in 87 (76%) of 115 enuretic children (of whom 60 with secondary nocturnal enuresis) after surgical removal of adenoid hypertrophy [24]. Four children constitute (57.1%) they had symptom of UTI of abdominal pain, frequency, urgency proved by GUE. In a study done in Jordan 5% of secondary enuresis have UTI as a cause of return bed wetting. Diabetes mellitus is considered one of medical illness that cause secondary nocturnal enuresis in our study 1 (2.2%) known case of newly diagnosed diabetes has nocturnal enuresis. In study done in Turkey in primary school found that 10% of secondary nocturnal enuresis has DM [25]. About psychological causes: Secondary nocturnal enuresis is significantly associated with stress. Researchers find that moving to a new town, parent conflict or divorce, arrival of a new baby, or loss of a loved one can cause insecurity, contributing to bed wetting [26].
In this study 38 (84.5%) of children secondary nocturnal enuresis is associated with psychological problems, of them 14 (31.1%) post stressful condition, 8 (17.8%) after immigration from their houses, 6 (13.3%) had history of death of one member in family, 4 (8.9%) have history of one of the family arrested in front of them, 3 (6.7%) Birth of new baby in family and 3 (6.7%) Separation between parents happened. In study by Alex Iglesias found significant relationship between secondary diurnal and nocturnal enuresis in study done on children after a car accident as a stressful condition. In another study done in New Zealand children for secondary enuresis at age of 10 years, analysis suggested that the child's level of exposure to adverse life events was associated with the onset of secondary enuresis, as children who were exposed to four or more stressful life events in a given year were 2.56 times more likely to develop secondary enuresis in that year [27]. Among 45 children with secondary nocturnal enuresis 8 of them (17.8%) have been punished by their family while 37 (82.2%) reinforced and reassured by their family to control themselves. In compartment with studies done in the United States, about 25% of enuretic children are punished for wetting the bed [28]. In Hong Kong, 57% of enuretic children are punished for wetting [29]. In study done in Germany at 1990 (14.3%) of secondary enuresis were reported to be punished. About self-esteem: Of the 45 child with secondary nocturnal enuresis, 27 (60%) had Social embarrassment, anxious, feel different from other and had more inferiority feeling. Theunis et al. reported that nocturnal enuresis has important negative effects on the self-esteem of children, which improved with successful treatment of enuresis also in another study done in finish population by Moilanen, the children with enuresis showed significant difference that they were more fearful, more impatient, and more anxious and had more inferiority feeling [30].
Conclusion
This study had shown that secondary nocturnal enuresis greatly affect school children, following traumatic stressful conditions, immigration from their houses, death in family, one of the family arrested, birth of a new baby, family problems like divorce, or others emotional or traumatic event. Girls were slightly more affected, the children with secondary enuresis were embarrassed, anxious and of low self-esteem. They were reinforced and reassured rather than punished by the parents.
References
- Elder JS, Behrman RE, Kliegman RM, et al. Voiding dysfunction nelson textbook of pediatrics 2007; pp: 2249-2253.
- Mellon M, Mcgrath L. Empirically supported treatments in pediatric psychology: Nocturnal Enuresis. J Pediatr Psychol 2000; 25(4): 193-214.
- Kevin L. Bed wetting and its treatment: Medical memo 2006; 10(1): 296-299.
- Hjalmas K, Arnold T, Bower W. Nocturnal enuresis: An international evidence based management strategy. J Urol 2004; 171: 2545-2561.
- Gontard A, Lehmkuhl G. Clinical behavioral problem in day and night wetting children. Pediatr Nephrol 1999; 13: 662-7.
- Neveus T, Tuvemo T, Lackgren G. Bladder capacity and renal concentrating ability in enuresis: Pathogenic implications. J Urol 2001; 165:2022.
- Fergusson D, Horwood LJ. Enuresis in children: Brazilian J Urol 2002; 28(3): 232-249.
- Cinar, U Vural C, Akir B, Topuz E, Turgut S, et. al. Nocturnal enuresis and upper airway obstruction. Int J Pediatr Otorhinolaryngol 2001; 59: 115-118.
- Redsell SA, Collier J. Bedwetting, behavior and self-esteem. A review of the literature. Child Care Health Dev 2001; 27(2):149-155.
- Cadwell P. Bedwetting and toilet training problems in children. Med J Aust 2005; 182(4): 190–192.
- Gontard V. Pediatric and child psychiatric perspective: Child psychiatry.1998; 39(5): 439-445.
- Glazener CMA. Simple behavioral and physical interventions for nocturnal enuresis in children. 2004.
- Evans J. Evidence based paediatrics: Evidence based management of nocturnal enuresis. BMJ 2001.
- Howard J, Benet M. Nocturnal enuresis bedwetting in older children: National Association for continence.
- Glazener CMA, Evans RE. Drugs for nocturnal enuresis in children. 2004.
- Glazener CMA, Evans RE. Tricyclic and related drugs for nocturnal enuresis in children: The Cochrane Database of Systematic Reviews. 2004.
- Lane M, Alexander K, Robert V. Primary and secondary nocturnal enuresis: Similarities in presentation. Pediatrics 2005; 115(4): 956-959.
- Alex I, Adam I. Secondary diurnal enuresis treated with hypnosis: A time-series design. Int J Clin Exp Hypn 2008; 56(2): 229-240.
- Asrashed k, Bataineh H. Frequency of enuresis in (5-10) year old children in Tafila, Jordan. Shiraz Med J 2007; 8(1): 53-40
- Pashapour N, Golmahammadlou S, Mahmoodzadeh H. Nocturnal enuresis and its treatment among primary-school children in Oromieh, Islamic Republic of Iran. East Mediterr Health J 2008; 14 (2):245-252.
- Unalack M. Enuresis nocturna: prevalence and risk factors among school age children in northwest Turkey. Eur J Gen Med 2004; 1: 21-25.
- Abdulazim M. Mabrouk E. Prevalence and correlates of nocturnal enuresis in the United Arab Emirates: Saudi Med J 2003; 24(1): 49-51.
- Sousa A, Kapoor H, Jagtap J, et al. Prevalence and factors affecting enuresis amongst primary school children. Indian J Urol 2007; 23: 354-357.
- Weider DJ, Sateia MJ, West RP. Nocturnal enuresis in children with upper airway obstruction: Otolaryngology Head Neck Surgery 1991; 105(66): 427-432.
- Unalack M. Enuresis nocturna: Prevalence and risk factors among school age children in northwest Turkey. Eur J Gen Med 2004; 1:21-25.
- Glazener CM, Evans JH, Peto RE. Treating nocturnal enuresis in children: Review of evidence. J Wound Ostomy Continence Nurs 2004; 31(4): 223-234.
- Fergusson D, Horwood T, Shannon F. Secondary enuresis in a birth cohort of New Zealand children. Paediatr Perinat Epidemiol 2008; 4(1): 53-63
- Evans D, Radunovich L. Bedwetting. University of Florida IFAS Extension.
- Wong S. Primary nocturnal enuresis: Patient attitudes and parental perceptions. Hong Kong J Paediatr 2004; 9: 54-58.
- Theunis M, Hoecke E, Paesbrugge S. Self-image and performance in children with nocturnal enuresis: Pediatric Urology 2002; 41(5): 660-667.