Research Article - Current Pediatric Research (2022) Volume 26, Issue 5
A retrospective study of pneumonectomy: Review of 100 cases in Al-Hussein teaching hospital/Thi-Qar (2013-2020).
Ali Al-Ghuzey*, Ahmed Abdulameer Daffar, Rafid Remthan Hussein Al-Temimi, Enass Mahdi saleh, Halah Ghalib
Department of Cardiovascular Surgery, University of Baghdad, Baghdad, Iraq
- Corresponding Author:
- Dr. Ali Al-Ghuzey
Department of Cardiovascular Surgery
University of Baghdad
Baghdad
Iraq
E-mail: alisaadoon755@gmail.com
Received: 03-Jan-2022, Manuscript No. AAJCP-22-51172;
Editor assigned: 05-Jan-2022, PreQC No. AAJCP-22-51172 (PQ);
Reviewed: 19-Jan-2022, QC No. AAJCP-22-51172;
Revised: 03-Mar-2022, Manuscript No. AAJCP-22-51172 (R);
Published: 10-Mar-2022, 10.35841/0971-9032.26.5.1427-1432.
Citation: Al-Ghuzey A, Daffar AA, Al-Temimi RRH, et al. A retrospective study of pneumonectomy: Review of 100 cases in Al-Hussein teaching hospital/Thi-Qar (2013-2020). Curr Pediatr Res 2022;26(5): 1427-1432.
Abstract
Background: Pneumonectomy is defined as the surgical removal of the entire lung. Pneumonectomy was first performed in 1933 by Evarts A. Graham for lung carcinoma. Indications for pneumonectomy can be broadly classified into malignant and non-malignant lung disease. Pneumonectomy is usually performed through a posterolateral thoracotomy incision as it provides the best exposure. Materials and Methods: A retrospective analysis was conducted in 100 patients who underwent pneumonectomy for different indications over a period of 9 years from May 2013 till May 2021 in Thi-Qar governorate. On admission, an informative history was taken from every patient including age, gender, onset and nature of clinical features related to disease itself . Other data included possible chronic diseases, presence of previous surgical operation and history of drug allergy and complications following surgery. Results: Males were affected slightly higher than females (55%). The ages affected ranged from less than 10 years to more than 60 years. Regarding the presentation, 60% of the patients suffered from cough and significant number of our patients (50%) had anorexia and fever. Perioperative complications included sinus tachycardia and atelectasis (40%) while mortality was mainly due to fatal bleeding. Conclusion: Pneumonectomy is indicated mainly for malignant lung disease. Single lung is compatible with life. Bleeding is a major challenge during and after surgical procedure of pneumonectomy.
Keywords
Pneumonectomy, Lungs, Surgery, Chronic diseases.
Introduction
Pneumonectomy is defined as the surgical removal of the entire lung. Extrapleural pneumonectomy is an expanded procedure that also involves resection of parietal and visceral pleura, ipsilateral hemidiaphragm, pericardium, and mediastinal lymph nodes [1]. It is usually reserved for patients with advanced malignant lung disease and is usually coupled with radiation and chemotherapy to improve survival in such a group of patients.
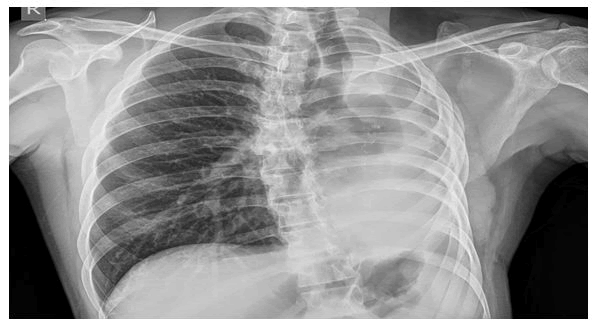
Pneumonectomy was first performed in 1933 by Evarts A. Graham for lung carcinoma. The patient, who was a 48 years old obstetrician, survived for a long period after the operation. Sarot described the first extrapleural pneumonectomy in 1949 [2-5]. It was initially used for the treatment of TB empyema but then became more commonly used for the treatment of mesothelioma (Figure 1).
Indications for pneumonectomy
Indications for pneumonectomy can be broadly classified into malignant and non-malignant lung disease. Malignancy constitutes the most common indication. It is usually reserved for patients with more advanced disease as when the tumor is located in the main stem bronchus or when it extends across a major fissure. Non-small cell lung cancer is the most common type of malignancy requiring pneumonectomy [6]. It is sometimes also indicated for mesotheliomas and extensive thymomas. Extension of the tumor into the carina will usually require sleeve pneumonectomy. Pneumonectomy is rarely performed for lung metastasis. Among the most common non-malignant conditions which require pneumonectomy are inflammatory lung disease.
In such a group of patients, underlying medical conditions should be properly optimized prior to proceeding for surgery. This includes the treatment of underlying infections, optimization of lung functions, and patients' nutritional status. Proper preoperative optimization decrease the risk of empyema and bronchopleural fistulas, which are frequent complications in such a group of patients [7-12]. Despite the challenges encountered, the outcome is usually favorable, and the chances of a complete cure are high. Another common indication for pneumonectomy is blunt and penetrating lung trauma causing major lung injuries as lacerations or tracheobronchial disruptions.
Contraindications
Unless it is an emergency, pulmonary function tests should be done before pneumonectomy to assess if the patient is fit for surgery. Forced Expiratory Volume in one second (FEV1) and diffusion capacity of the lung for carbon monoxide provide the most accurate risk estimates of postoperative morbidity and mortality. If the estimated postoperative FEV1 or DLCO is less than 40% of predicted, the risk of morbidity and mortality is quite high, and other functional assessment modalities should be sought of these modalities, cardiopulmonary exercise testing to measure maximal oxygen consumption (Vo(2) max) is the most important. A Vo(2) max less than 10 to 15 ml/kg/min is associated with an increased risk of postoperative complications. Stair climbing, shuttle walk test, and the 6-min walk test may also be considered, but data on the interpretation of the results of these tests are quite limited. Pneumonectomy is contraindicated in patients who are deemed not fit based on the above tests, and more conservative treatment modalities should be sought.
Materials and Methods
Cardiac risk assessment should also be performed, and other management strategies should be sought in patients with severe valvular disease, severe pulmonary hypertension, or poor ventricular function. Also, in patients with PET or CT scan evidence of tumor extension past the diaphragm to intra-abdominal structures or contralateral hemithorax or the ribs, surgery is prohibited.
Preparation
Preoperative evaluation of those patients is of paramount importance. This includes an anatomical and a detailed medical evaluation to assess the risk of postoperative complications properly This usually starts with pulmonary function testing, which includes spirometry, lung volume measurements, and diffusing capacity of lungs for carbon monoxide. FEV1 and DLCO provide the most accurate predictors of postoperative morbidity and mortality, as mentioned previously. They provide an indirect measurement of the pulmonary reserve. The calculation of predicted postoperative FEV1 and DLCO takes into account the preoperative values and measurements of lobar or whole lung contribution to function as measured by V/Q scanning or CT. This is done by subtracting the lung segments to be resected from the total lung function. It is also worth mentioning that baseline resting PO2 and PCO2 have not been proven to be as useful as a measurement of FEV1 and DLCO for assessing patient's eligibility for surgery. cardiac risk assessment with an EKG, echocardiography, or a stress test should be performed when deemed necessary. In patients with active or high-risk cardiac conditions, other treatment modalities should be sought.
Lung imaging with a CT or PET scan is usually required within 6 to 8 weeks of the planned surgery. A set of routine labs, including a complete blood count, renal function panel, and coagulation profile, is usually drawn. Of note, chronic kidney disease is associated with an increased risk of worsening kidney injury and mortality after pneumonectomy. A type and screen are usually obtained in anticipation of blood loss. Before the start of surgery, a thoracic epidural is sometimes placed to help with postoperative pain management. The patient is then usually positioned in a lateral decubitus position with the operating side up. Proper positioning of the Double Lumen Tube (DLT) or the bronchial blocker is usually reconfirmed with the FOB, and single lung ventilation is then started. Care should be taken to ensure proper positioning to avoid perioperative nerve injury
Technique
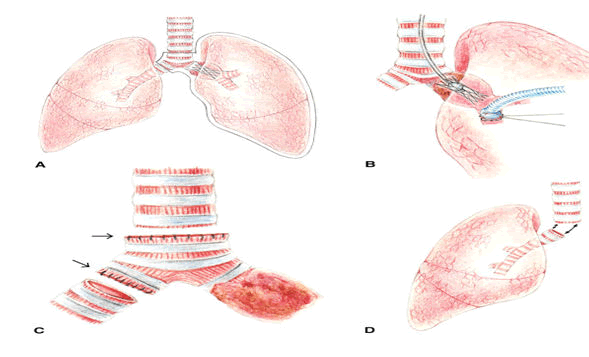
Pneumonectomy is usually performed through a posterolateral thoracotomy incision as it provides the best exposure. An incision is usually done at the level of the fourth or fifth intercostal space. Other approaches commonly used are the axillary and the anterior thoracotomy; however, they provide poor access to the posterior thorax. In the absence of severe hemodynamic instability and ongoing blood loss, a restrictive IV fluid strategy is usually employed. This is associated with a lower incidence of acute lung injury and enhanced recovery after surgery. Vasopressors are usually preferred over IV fluid boluses to correct hypotension associated with general anesthesia. A lung-protective ventilation strategy is usually employed to decrease the risk of acute lung injury. This includes the use of low tidal volumes of around 5 ml/kg of ideal body weight, maintenance of low airway driving pressure, and the use of PEEP. FiO2 should be kept at the lowest possible to keep arterial oxygen saturation above 90%. Unless contraindicated, permissive hypercapnia is usually allowed to achieve these goals. At the conclusion of surgery, two lung ventilation is resumed, and the patient is returned to the supine position. Bronchoscopy is done if needed. An arterial blood gas is usually drawn to ensure adequate oxygenation and ventilation, and the patient is extubated if deemed appropriate. Some patients may require Continuous Positive Airway Pressure (CPAP) or High Flow Nasal Cannula (HFNC) after extubation. If the patient is to remain intubated, DLT has to be changed for a single lumen tube using a tube exchanger catheter. Postoperative care is of great importance to decrease the incidence of complications (Figure 2).
Complications
Following pneumonectomy, pulmonary functions decrease but usually less than anticipated for removal of 50% of lung, especially for residual volume, and this may be explained by overexpansion of the remaining lung tissue. FEV1, FVC, DLCO, and lung compliance decrease. Airway resistance increases. Patients with no disease in the remaining lung usually do have normal SaO2, PO2, and PaCO2 at rest. A chest X-ray immediately following pneumonectomy usually shows the trachea in the midline and the postpneumonectomy space to be filled with air. Later, that space becomes filled gradually with fluid at a rate of 1-2 intercostal space/day. The ipsilateral diaphragm becomes elevated, and the mediastinum is gradually shifted towards the operative side. Resting heart rate typically increases, and stroke volume decreases, following pneumonectomy. Pulmonary artery pressure, pulmonary vascular resistance, and central venous pressure usually do not change. Cardiac function in long term survivors is usually compromised, and this may be explained by the altered position of the heart.
Following a pneumonectomy, the most common complications include
- Cardiac arrhythmias, one of the most common complications after pneumonectomy. Atrial fibrillation/flutter is the most common and usually occurs in the first three days following surgery.
- Postpneumonectomy cardiac herniation. It usually occurs within the first 24 hours after surgery, but it has been reported up to 6 months following pneumonectomy. The condition presents with an abrupt drop in blood pressure and hemodynamic collapse.
- Pulmonary complications like pneumonia, atelectasis, respiratory failure are also common. The incidence and severity of such complications increase with advanced age and may require reintubation and mechanical ventilation.
- About 1.5% to 4.5% of patients undergoing pneumonectomy will end up having a bronchopleural fistula. It is associated with a mortality of 29% to 79%. Risk factors include right-sided procedures, a large diameter bronchial stump, residual tumor, concurrent radiation or chemotherapy, age greater than 60 years, and prolonged postoperative mechanical ventilation. Symptoms include fever, cough, hemoptysis, subcutaneous emphysema. A persistent air leak is usually detected if a chest tube is still in place. A chest X-ray usually demonstrates a new air-fluid level or worsening of a preexisting air-fluid level. Management includes drainage of pleural space, systemic antibiotics. Surgical repair may be required in severe cases.
- Injury to the diaphragm, liver, spleen, or a major vessel is also one of the known complications.
- Postpneumonectomy pulmonary edema. It occurs in 2% to 5% of cases and typically presents on postoperative days 2 to 3 pneumonectomy, lymphatic damage and ventilator-induced lung injury.
- Other potential complications include multiorgan dysfunction, acute lung injury, Acute Respiratory Distress Syndrome (ARDS), postoperative acute kidney injury.
Patients and methods
This is a retrospective study of 100 cases underwent pneumonectomy due to multiple pulmonary diseases over a period of 9 years May 2013 till May 2021 in AL-Hussein teaching hospital in Thi-Qar governorate. On admission, an informative history was taken from every patient including age, gender, onset and nature of clinical features related to disease itself. Base line data include patient demographics like age, gender, presentations, complications and other possible chronic diseases, presence of previous surgical operation and history of drug allergy, etc. Different investigations done including chest X-ray, chest CT scan, routine blood investigations, renal functions, echocardiography, bronchoscopy. Most of our patients were selected randomly who previously did pneumonectomy due to multiple causes. Of course, a consent was taken from the patient and the family before the surgical procedure.
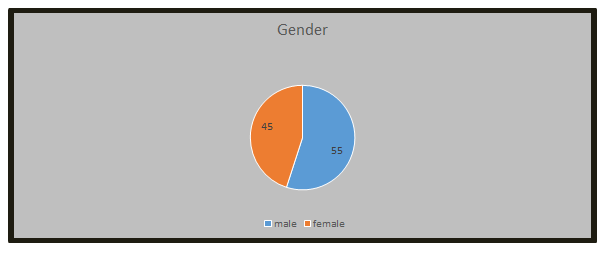
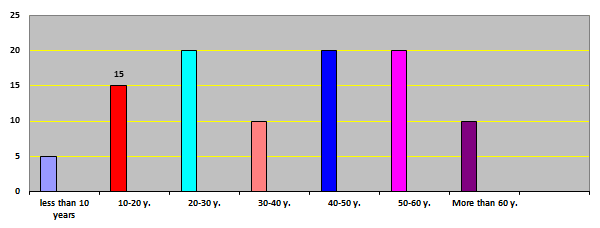
Results
Of the 100 cases of lung disease patients who underwent pneumonectomy, 55 of them were males and 45 females aged from less than 10 up to more than 60 and this sample was obtained from AL-Hussein teaching hospital. Every patient was exposed for clinical examination especially auscultation of chest. Different investigations were done including chest X-ray, chest CT scan and blood investigations, renal function test, electrocardiography, echocardiography, bronchoscopy (Figures 3,4 and Tables 1-3).
Table 1. Correlation of the patient's age with pneumonectomy.
| Age of patient | NO. of patient | Percentage |
|---|---|---|
| Less than 10 years | 5 | 0.05 |
| 10-20 years | 15 | 0.15 |
| 20-30 years | 20 | 0.2 |
| 30-40 years | 10 | 0.1 |
| 40-50 years | 20 | 0.2 |
| 50-60 years | 20 | 0.2 |
| More than 60 years | 10 | 0.1 |
| Total | 100 | 1 |
Table 2. Patient's presentations.
| Presentation | No. of Patients | Percentage |
|---|---|---|
| Cough | 60 | 0.6 |
| Dyspnea | 30 | 0.3 |
| Hemoptysis | 5 | 0.05 |
| Fever and anorexia | 50 | 0.5 |
| Wight loss | 30 | 0.3 |
| Chest pain | 10 | 0.1 |
Table 3. Represents the side of lung resected.
| Side of lung | No. of Patients | Percentage |
|---|---|---|
| Right lung | 55 | 0.55 |
| Left lung | 45 | 0.45 |
| Total | 100 | 1 |
Mortality occur during and after surgery, 2 of patients died during surgery due to bleeding and cardiac arrest, and one after surgery due to sepsis. Most complications were treated by conservative measures (Tables 4 and 5).
Table 4. Represents estimation of complications after surgery.
| Compications | No. of patient | Percentage |
|---|---|---|
| Infections | 15 | 0.15 |
| Bleeding | 10 | 0.1 |
| Sinus Tachycardia | 40 | 0.4 |
| Atrial fibrillation | 5 | 0.05 |
| Atelectasis of other lung | 40 | 0.4 |
Table 5. Indications for pneumonectomy.
| Indication for pneumonectomy | No. of patients | Percentage |
|---|---|---|
| Ca lung (non small cell carcinoma) | 60 | 0.6 |
| Carcinoid | 20 | 0.2 |
| Bronchiectasis | 2 | 0.02 |
| Lung Hydatid cyst | 2 | 0.02 |
| Trapped lung syndrome for chronic empyema | 2 | 0.02 |
| Massive heamoptasis | 2 | 0.02 |
| Extra pulmonary tumor with invation of lung | 2 | 0.02 |
| Lobar emphysema | 2 | 0.02 |
| Giant bullea | 2 | 0.02 |
| Trapped lung for bronchopleural fistula | 2 | 0.02 |
| Damaged lung due to previous TB | 4 | 0.04 |
| Total | 100 | 1 |
Discussion
In this analysis there were Fifty five patients males and fourty five patient females and both genders nearly equal with slight higher in males, in contrast to Pneumonectomy in the Indian scenario-a review of current indications and results, there were seventy four patient with male to female ratio 2:1. Morever, all ages did pneumonectomy but the third, 5th and 6th decades were exposed more than other age groups, however this differs from Indian study [13]. The number of children was 6 cases in Indian study (8.1%) but children in our study was 5 (5%).
Cough was the most common presentation among our patient (60%) which might be due to many pulmonary diseases like infections (abscess, tuberculosis, bronchiectasis, etc), benign tumors or cancers [14-16], however the most common indication was cancer (non small cell carcinoma) and this didn’t agree with Pneumonectomy in the Indian scenario-a review of current indications and results where Post-tuberculosis-destroyed lung was the predominant indication (43.24%). While this indication in our study was done for four cases (4%). However the most common indication is cancer according to NCBI book.
Right pneumonectomy is slightly more than left (55%) that could be due to multiple reasons like relation of it to liver (hydatid), site of aspiration (abscess), cancers whereas in that study. Left pneumonectomy was performed in 48 patients (64.86%). Complications occurred in form of respiratory (atelectasis) and cardiac (sinus tachycardia) as most likely complications (40 cases, 40%), while in indian study, post-operative complications encountered were reactionary hemorrhage (1), empyema (2), bronchopleural fistula (1), and chylothorax.
To a lesser extent infection also occured in (15%) and bleeding (10%) most of it resolved spontaneously. Mortality was recorded in our study, one of them died because of bleeding during surgery, one case due to cardiac arrest and one case postoperatively due to sepsis, but this fact does not agree with indian study were one early post-operative death occured due to fulminant respiratory failure [17]. Early mortality rate was 1.35%. early mortality rate in our study was 3%. Prognosis was good in uncomplicated cases and in benign complications that treated conservatively.
Conclusion
- Males were exposed for pneumenectomy more than females.
- Third, fifth and sixth decade mostly did pneumonectomy.
- Cough was the most common presentation before surgery.
- Right pneumonectomy was done more than left pneumonectomy.
- Cardiac and respiratory complications occurred during and after surgery
- 3 mortality cases were recorded.
- Cancer was the most common indication for pneumonectomy.
- Patients may live normal life span after pneumonectomy.
Recommendations
- Sophisticated investigations may be mandatory for persistent respiratory symptoms in order to detect lung pathologies which may have an indication for surgery.
- Early diagnosis of lung cancer if very important in order to improve prognosis after pneumonectomy.
- Good preoperative preparation is crucial to prevent unwanted complications during and after surgery.
- Careful monitoring during and after surgery may decrease morbidity and mortality.
- Conservative measures may treat most complications during and after surgery.
References
- Casiraghi M, Maisonneuve P, Brambilla D, et al. Induction chemotherapy, extrapleural pneumonectomy and adjuvant radiotherapy for malignant pleural mesothelioma. Eur J Cardiothorac Surg. 2017;52:975-81. [Crossref][Google Scholar][Pubmed]
- Brunelli A, Kim AW, Berger KI, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:166-190. [Crossref][Google Scholar][Pubmed]
- Colice GL, Shafazand S, Griffin JP, et al. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines (2nd edition). Chest. 2007;132:161-77. [Crossref][Google Scholar][Pubmed]
- Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll Cardiol. 2007;50:1707-32. [Crossref][Google Scholar][Pubmed]
- Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann Intern Med. 2006;144:581-95. [Crossref][Google Scholar][Pubmed]
- Mathew A, Devereaux PJ, O'Hare A, et al. Chronic kidney disease and postoperative mortality: A systematic review and meta-analysis. Kidney Int. 2008;73:1069-81. [Crossref][Google Scholar][Pubmed]
- Alam N, Park BJ, Wilton A, et al. Incidence and risk factors for lung injury after lung cancer resection. Ann Thorac Surg. 2007;84:1085-91. [Crossref][Google Scholar][Pubmed]
- Vincent JL, De Backer D, Wiedermann CJ. Fluid management in sepsis: The potential beneficial effects of albumin. J Crit Care. 2016;35:161-7. [Crossref][Google Scholar][Pubmed]
- Licker M, Diaper J, Villiger Y, et al. Impact of intraoperative lung-protective interventions in patients undergoing lung cancer surgery. Crit Care. 2009;13:41. [Crossref][Google Scholar][Pubmed]
- Roceto Ldos S, Galhardo FD, Saad IA, et al. Continuous Positive Airway Pressure (CPAP) after lung resection: A randomized clinical trial. Sao Paulo Med J. 2014;132:41-7. [Crossref][Google Scholar][Pubmed]
- Smulders SA, Holverda S, Vonk-Noordegraaf A, et al. Cardiac function and position more than 5 years after pneumonectomy. Ann Thorac Surg. 2007;83:1986-92. [Crossref][Google Scholar][Pubmed]
- Amar D. Postoperative atrial fibrillation: Is there a need for prevention?. J Thorac Cardiovasc Surg. 2016;151:913-5. [Crossref][Google Scholar][Indexing at]
- Frendl G, Sodickson AC, Chung MK, et al. 2014 AATS guidelines for the prevention and management of perioperative atrial fibrillation and flutter for thoracic surgical procedures. J Thorac Cardiovasc Surg. 2014;148:153-93. [Crossref][Google Scholar][Pubmed]
- Keshava HB, Boffa DJ. Cardiovascular complications following thoracic surgery. Thorac Surg Clin. 2015;25:371-92. [Crossref][Google Scholar][Pubmed]
- Yano T, Kawashima O, Takeo S, et al. National hospital organization network collaborative research-thoracic oncology group. A prospective observational study of pulmonary resection for non-small cell lung cancer in patients older than 75 years. Semin Thorac Cardiovasc Surg. 2017;29:540-547. [Crossref][Google Scholar][Pubmed]
- Darling GE, Abdurahman A, Yi QL, et al. Risk of a right pneumonectomy: Role of bronchopleural fistula. Ann Thorac Surg. 2005;79:433-7. [Crossref][Google Scholar][Pubmed]
- Karuppannan M, Ravinutala VK, Tella RKD, et al. Pneumonectomy in the Indian scenario: A review of current indications and results. Indian J Thoracic Cardiovasc Surg. 2015;31:218-223.