Case Report - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 3
A rare case of third nerve palsy in acquired immune deficiency syndrome
Harshini Rajula1*, Nanda L1, Kaushal Kumar1, Nidhi Chandrakar2, Anil Kumar Shukla21Department of Ophthalmology, Rajarajeswari Medical College, Bangalore, Karnataka, India
2Department of Radiology, Rajarajeswari Medical College, Bangalore, Karnataka, India
- Corresponding Author:
- Dr. Harshini Rajula
Department of Ophthalmology Rajarajeswari
Medical College Bangalore, Karnataka India
E-mail: harshinirajula@gmail.com
Citation: Rajula H, Nanda L, Kumar K, et al. A rare case of third nerve palsy in acquired immune deficiency syndrome. J Clin Ophthalmol 2020;4(3): 269-272.
Accepted: July 14, 2020
Abstract
A male aged 40 years was presented with double vision and blurring of vision persisting for past one week. He is known case of Hospital where he was admitted and treated for tuberculosis. He was detected retro-positive six months earlier was not on anti-retroviral therapy. His BCVA was 6/9(p) in both eyes. Left eyelid was with partial ptosis present and pupil was mid dilated, non-reacting to light. It was also noticed restriction of adduction, elevation and depression in left eye. Right eye EOM was full and normal. Vertical crossed diplopia was present. Fundus examination revealed tessellated background in both eyes. MRI (contrast) revealed inflammatory etiology to be considered as Toxoplasmosis. It was estimated that Neuro-Ophthalmic manifestations occur in 2%-8% of Human Immune Deficiency Virus (HIV) infected patients. Toxoplasmosis could be a cause of third nerve palsy in HIV infected patient.
Keywords
Human Immune Deficiency Virus (HIV), Third nerve, Toxoplasmosis.
Introduction
The estimated annual number of new HIV infection in 2018 is 1.7 million world-wide. The Human Immune Deficiency Virus (HIV) remains public health problem in developing countries. Neuro-ophthalmic involvement has been widely described in HIV asymptomatic patients and in those with full blown AIDS. Ocular cranial nerve palsies occur in 4% of patients with AIDS [1].
Oculomotor nerve injuries are located at different points of its course and its anatomical relationship of various portions is responsible for its clinical features. In the developing countries people with HIV infection are more prone to infection like toxoplasmosis, tuberculosis, cytomegalovirus, varicella zoster and progressive multifocal leuco-encephalopathy. Hamed et al. reported ocular motility manifestations of focal brainstem dysfunction as clinical features in three patients with HIV infection [2].
We report an interesting case of third nerve palsy in HIV positive patient.
Case History
A male patient aged 40 years was presented with double vision and blurring of vision present throughout the day, in all directions, disappears by closing one eye, history of drooping of left upper eyelid for the past one week with no diurnal variation. Patient had admitted at the Hospital 5 years ago with history of pulmonary tuberculosis disease and undergone treatment for 6 months. Later, six months back he presented with fatigue and weakness and was detected retro-positive. The treatment was commenced but the patient discontinued.
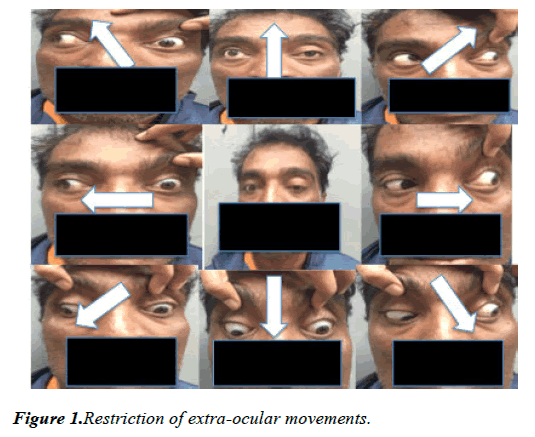
On examination it was found that his visual acuity at 6/9, near vision N6 in both the eyes, moderate ptosis with poor levator palpebrae superioris, good bells phenomenon and reduced vertical palpebral fissure. Left eye adduction, elevation and depression were restricted (Figure 1). Pupil was round, 5mm non-reacting to light in the left eye. Rest of the anterior segment was normal on slit lamp examination. Fundus examination revealed tessellated background. Vertical crossed diplopia was found. Intraocular pressure was normal in both the eyes.
Patient was moderately built and oriented. No focal neurological deficit except for dropping of left upper eyelid on first day of the visit. Rest of the systemic examination was normal. Patient was advised for radiological investigations and for symptomatic treatment, patching of left eye was done. Serology for HIV antibodies was repeated.
Course of illness
Later, after a week patient presented with gradual progression of ptosis on left side, further diminution of vision, numbness in right palm and weakness in right upper and lower limb. Urgent MRI Brain with contrast and cluster of differentiation 4(CD4) cell count was advised. His serology of HIV antibodies was reactive by coombs test. Physician reference was given.
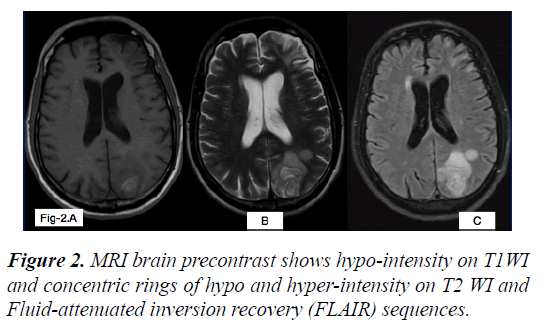
MRI brain (Pre-contrast) shows hypo-intensity on T1WI and concentric rings of hypo and hyper-intensity on T2 WI and Fluid-attenuated inversion recovery (FLAIR) sequences (Figure 2).
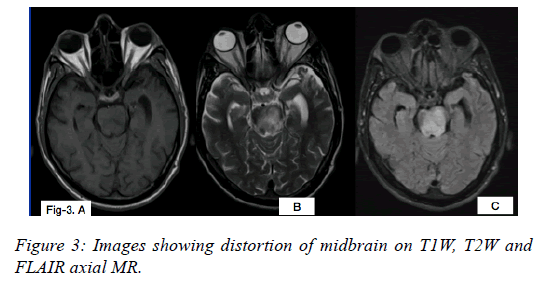
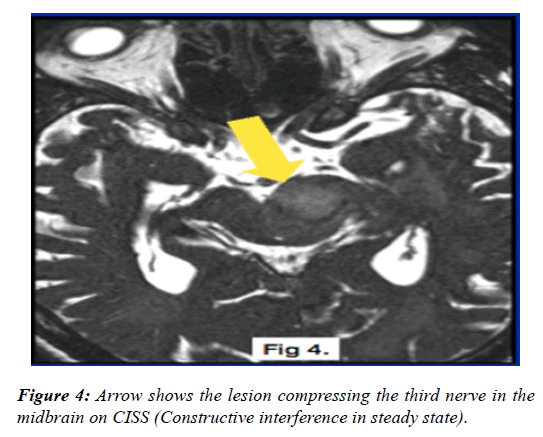
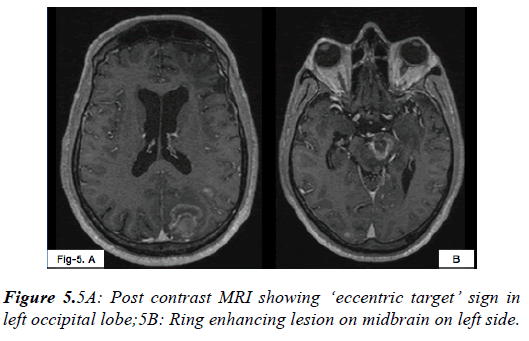
From the MRI report features suggested of HIV encephalopathy with toxoplasmosis infection (Figures 3-5).
Chain of Events:
• On first day of the visit patient presented with double vision and drooping of left upper eyelid. He revealed his HIV status while performing clinical evaluation. MRI brain (contrast) was advised and left eye patching was done for diplopia.
• A week later patient with confirmed HIV antibodies positive status presented with gradual progression of ptosis on left side, further diminution of vision, numbness in right palm and weakness in right upper and lower limb. Urgent MRI brain (contrast) which was not done earlier, CD4 cell count and physician reference was advised.
• Physician advised for admission but due to financial constraints patient refused and was referred to higher center.
• After a week, patient was brought to emergency room unconscious, not responding to verbal or painful stimuli and was referred to higher center.
• After two days we lost the patient.
Discussion
Oculomotor nerve has two major components. Parasympathetic fibers which supply ciliary muscles and sphincter pupillae.Inner somatic fibers that supply superior, middle, inferior recti, inferior oblique and levatorpalpebraesuperioris (LPS).Anatomically divided into nuclear, fasicular, subarachnoid space, cavernous sinus and the orbital portion. Lesions at nuclear level are rare and cause partial palsy. Fascicles consist of efferent fibers and travel through red nucleus, medial aspect of cerebral peduncles and emerge from midbrain and pass into inter-peduncular space. Syndromes associated with this are as follows:
• Benedikt syndrome: Ipsilateral third nerve palsy and contralateral tremors
• Weber syndrome: Ipsilateral third nerve palsy and contralateral hemiplegia
• Nothnagel syndrome: Ipsilateral third nerve palsy and cerebellar ataxia
• Claude syndrome: Features of both benedikt and Nothnagel syndromes.
Subarachnoid portion is the most common site of an isolated oculomotor paresis. Aneurysm of posterior communicating artery, extra-dural and sub-duralhaemorrhage following head trauma are associated with third nerve palsy.
In the cavernous sinus the third nerve pierces the dura lateral to posterior clinoid process causing third, fourth, sixth and the first division of trigeminal nerve paralysis. In the anterior part of cavernous sinus, third nerve divides into superior and inferior branches. Lesion in the inferior division presents with limitation of adduction and depression.
Surgical lesion like aneurysms, trauma, uncal herniation causes pupil involvement by compressing pial blood vessels and superficially located pupillary fibers. Medical lesion such as hypertension, diabetes causes no pupil involvement.
Signs of third nerve palsy are:
• Ptosis due to paralysis of LPS muscle.
• “Down and out” position of the eye due to unopposed action of lateral rectus and superior oblique muscles
• Diplopia occurs due to deviation of affected eye resulting in image falling on extra-foveal point.
• Pupil dilation and defective accommodation due to parasympathetic palsy.
Evaluation of patient with pupil involvement in third nerve palsy includes MRI for intracranial lesion. CT angiography should be performed urgently if clinical features are suspicious of aneurysm. Patients with pupil-sparing third nerve palsy laboratory investigations includes blood pressure, complete blood picture, blood sugar levels, glycatedhaemoglobin (Hb1AC) and erythrocyte sedimentation rate (ESR).
Evaluation of patient with pupil involvement in third nerve palsy includes MRI for intracranial lesion. CT angiography should be performed urgently if clinical features are suspicious of aneurysm. Patients with pupil-sparing third nerve palsy laboratory investigations includes blood pressure, complete blood picture, blood sugar levels, glycatedhaemoglobin (Hb1AC) and erythrocyte sedimentation rate (ESR).
The prevalence of neuro-ophthalmic manifestations in patients with HIV cases regardless of the presence of neurological symptoms, has been reported to range between 3% and 8% [4,5]. In series reported by Helweg-Larsen et al only 17 of 589 patients with neurological manifestations (3%) had ocular nerve palsy [6].
Neurologic sequel of the disease leads to much of the morbidity and mortality of AIDS. Toxoplasma gondii is one of the most prevalent opportunistic central nervous system infections in immune-compromised patient [7]. Clinical features of toxoplasma encephalitis include headache, fever, hemiparesis, ataxia, cranial nerve palsy, chorea, rigidity, seizures. In ocular toxoplasmosis retinal scars, vitritis, retinal detachment and optic neuritis may occur [8]. Mwanza et al. reported 11 HIV infected patient with toxoplasmosis, among whom 4 cases had 3rd cranial nerve palsy and 7 had 6th cranial nerve palsy [1]. Pillay S et al. reported 22 cases of cranial nerve deficiency in HIV-infected patients, and only one patient was definitively diagnosed with toxoplasmosis [9].
MRI has an important role in differentiation of cerebral lesions. A concentric target sign on T2WI weighted images with concentric hyper-intense and hypo-intense zones is more specific for cerebral toxoplasmosis.
The standard treatment for toxoplasmosis in HIV is sulfadioxine and pyrimethamine with leucovorin as needed for a minimum of 4-6 weeks. Alternate therapeutic regimens include clindamycin in combination with pyrimethamine; atovaquone plus pyrimethamine; and azithromycin plus pyrimethamine plus rifabutin. Relapses are common, and patient with history of prior toxoplasmic encephalitis receive maintenance therapy with sulfadiazine, pyrimethamine, and leucovorin as long as their CD4+T cells remain less than 200 cells/ul [10].
The patient was positive for HIV anti-bodies which lead to impaired of immune function. The MRI report showed multiple ill-defined lesions in the left frontal and temporal lobes, bilateral parietal and occipital lobes, left basal ganglia, midbrain, thalamus and posterior portion of pons which are hypo-intense on T1 and concentric bands of hypo and hyperintensity on T2, FLAIR sequences. A lesion involving midbrain on the left side with involvement of left oculomotor nerve explains isolated third nerve palsy secondary to focal lesion. Multiple heterogenous signal intensity lesions showing heterogeneous post-contrast enhancement (“eccentric target” sign) with few areas of diffusion restriction in the mentioned areas are suggestive of HIV encephalopathy with toxoplasmosis infection. Henceforth the patient was referred to higher center for further evaluation and CD4 cell count. Patient being noncompliant had multiple visits to different hospitals because of the progression of disease severity. We lost the patient after a week.
HIV related stigma is key issue that impacts people living with HIV. Stigma and discrimination in the family, community as well as clinics are the significant barriers to HIV treatment which lead to negative consequences and poor adherence to medication in the patient.
Conclusion
It is strongly concluded that isolated third nerve palsy secondary to HIV encephalopathy due to focal lesion of cerebral toxoplasmosis is a rare clinical presentation and also based on an extensive search of reported literature on the related cases.
References
- Mwanza JC, Nyamabo LK, Tylleskär Tet al. Neuro-ophthalmological disorders in HIV infected subjects with neurological manifestations. Br J Ophthalmol. 2004;88:1455-9.
- Hamed LM, Schatz NJ, Galetta SL. Brainstem Ocular motility defects and AIDS. AmJ Ophthalmol.1988;106:437-42.
- Brad Bowling. Kanski’s Clinical Ophthalmology A systematic approach, 8th ed, Elsevier; 2016:821-825.
- Woods AD, Caputo MK. Neuro ophthalmic manifestations of AIDS. Optom Clin.1996;5:113-52.
- Mansour AM. Neuro-ophthalmic findings in acquired immunodeficiency syndrome. J Clin Neuro ophthalmol.1990;10:167-74.
- Helweg-Larsen S, Jakobsen J, Boesen F, et al. Neurological complications and concomitants of AIDS. ActaNeurol Scand.1986;74:467-74.
- Luft BJ, Brooks RG, Conley FK,et al. Toxoplasmic encephalitis in patients with the acquired immune deficiency syndrome. JAMA. 1984;252:913-7.
- Delair E, Latkany P, Noble AG, et al. Clinical manifestation of ocular toxoplasmosis. OculImmunolInflamm. 2011;19:91-102.
- Pillay S, Ramachandre K. Audit of computed tomography brain findings in HIV-infected patients with space occupying infective lesions at a regional level hospital in KwaZulu-Natal. SAGE Open Med. 2018;6:2050312118801242.
- Anthony S Fauci, Gregory K Folkers, H.Clifford Lane. Human Immunodeficiency Virus: AIDS and Related Disorders . Harrison’s principles of internal medicine, 20th ed, McGraw-Hill Education; 2018:1393-1445.