Case Report - Journal of Clinical Ophthalmology (2018) Volume 2, Issue 2
A rapidly growing periorbital mass: pilomatrixoma.
Minji Ha1*, Mee Yon Lee1, Su Young Kim2, Young Chun Lee1 and Hye Young Shin1
1Department of Ophthalmology & Visual Science, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea
2Department of Pediatrics, Pusan National University Children’s Hospital, Pusan, Korea
- *Corresponding Author:
- Minji Ha Department of Ophthalmology & Visual Science
Seoul St. Mary’s Hospital, College of Medicine
The Catholic University of Korea
Seoul, South Korea
Tel: 82-10-2989-5252
E-mail: ddanglee@gmail.com
Accepted date: October 22, 2018
Citation: Ha M, Lee MY, Lee YC, et al,. A rapidly growing periorbital mass: pilomatrixoma. J Clin Ophthalmol 2018; 2(2):101-103.
DOI: 10.35841/clinical-ophthalmology.2.2.101-103
Visit for more related articles at Journal of Clinical OphthalmologyAbstract
Purpose: To report a case of pilomatrixoma that presented as a periorbital area painful, perforating, rapidly growing mass. Case summary: A 35-year-old man presented with rapidly growing a left lower periorbital mass 5 months duration. On examination, it measured 13 mm sized and it was located at the lateral side of the left lower periorbital area. The mass was accompanied with pain. A perforation with yellowish crust on the left lower periorbital area was observed. Conclusion: In patients presenting with a painful and perforating mass, the pilomatrixoma should be considered as a differential diagnosis of a solitary periorbital mass.
Keywords
Eyelid, Pilomatrixoma, Periorbital mass, Ultrasound bio microscopy, Anucleate squamous cells, Epithelial tumor
Case Report
Eyelid pilomatrixoma is a rare benign neoplasm originating from the matrix of the hair root. It was first reported by Malherbe and Chenantais in 1880 as "calcifying epithelioma" and was thought to be derived from the sebaceous gland [1]. Clinically, the lesion is characterized by slow growth, firm, non-tender, subcutaneous nodule, and is adherent to the skin. It is also known that pilomatrixoma is typically not caused by trauma or inflammation. We report for the first time a rare case of a periorbital pilomatrixoma accompanied by rapidly growth, perforation, and pain.
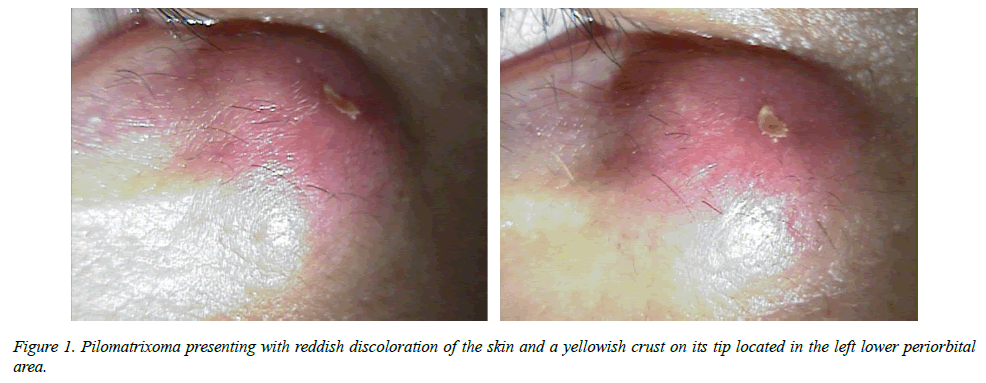
A 35-year-old man presented with a rapidly growing left lower periorbital mass of 5 months’ duration. There was a tiny palpable mass at the same location. The patient denied any history of previous inflammation or major trauma at the site except for frequent rubbing on the lesion. Physical examination revealed a round and nodular mass with a size of 13 mm located in the left lower periorbital area. The mass showed red discoloration, was hard and fixed to the skin. It presented tenderness. Perforation with a yellowish crust on the left lower periorbital area was observed (Figure 1).
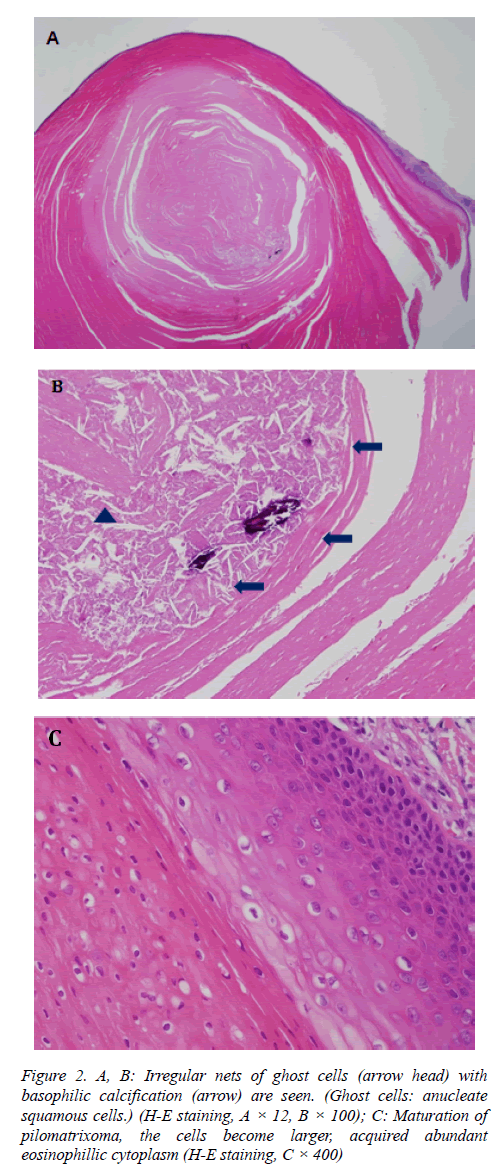
The tumor was solid and yellowish, was covered by a thick capsule, and measured 13 mm in size. Histopathology showed characteristic irregular nets of ghost cells with basophilic calcification (Ghost cells: anucleate squamous cells.) Among them, multinucleated giant cells with chronic inflammatory infiltrates were also seen (Figure 2). There was no recurrence of the tumor until 11 months after surgery.
Figure 2: A, B: Irregular nets of ghost cells (arrow head) with basophilic calcification (arrow) are seen. (Ghost cells: anucleate squamous cells.) (H-E staining, A × 12, B × 100); C: Maturation of pilomatrixoma, the cells become larger, acquired abundant eosinophillic cytoplasm (H-E staining, C × 400)
Pilomatrixoma can occur in any age group, but it is known to occur in teens and between ages of 50-60 years [2,3]. It can occur almost anywhere on the body, but it has a propensity to occur in the head and neck region, often involving the eyelid or the eyebrow. Clinically, pilomatrixoma is hard, painless, and appears as a solitary subcutaneous nodule with a clear border and an area of 5 to 30 mm in size. [4] Histologically, pilomatrixoma is an epithelial tumor composed of irregularly shaped epithelial islets, and two types of cells are present. The first type of cells are nucleus basal cells arranged along the island-shaped periphery, and the second type of cells are anucleate eosinophilic cells (so- called ghost cells or shadow cells) located in the center of the island [2].
The tumor is typically known to grow slowly over several months or years. There are usually no symptoms. But pain is caused by inflammation of the mass or ulceration. In adults, it is necessary to differentiate this lesion from benign tumors of the hair follicle origin. When the mass shows rapid growth, it is necessary to differentiate it from malignant tumors such as basal cell carcinoma and metastatic carcinoma. In our case, the tumor had grown rapidly and it presented as a crust lesion in the center. The different unusual morphological presentations of pilomatrixoma make its clinical diagnosis difficult. A definite diagnosis of pilomatrixoma can only be established after excision and histologic examination.
Perforating pilomatrixoma is a rare variant of pilomatrixoma. Periorbital pilomatrixoma, which is associated with pain and perforation, has not yet been reported. Pilomatrixoma reported in this case showed a sudden increase in its size without a major trauma history, but after frequent rubbing on the mass. The mass was small in size before rubbing. The mechanism of perforation of pilomatrixoma is still unknown. Mehregan proposed that perforation of the epidermis is accomplished by means of the biological phenomenon of transepithelial elimination; i.e., foreign material, such as calcium salts and bony tissue, acts as a mechanical irritant and it is eliminated from the skin surface through the epidermis or the hair follicle [5]. Our case shows atypical clinical features as the mass showed tenderness and a yellow crust in the center with recent perforation. The rapidly increasing mass and perforation might be due to mechanical irritation of the prior small mass.
In conclusion, pilomatrixoma should be suspected in any young adult patient who has a firm, perforated mass with tenderness in the lower periorbital area. Characteristic clinical findings can help clinicians to differentiate this lesion from other tumors.
References
- Malherbe A, Chenantais J. Note sure L’epitheliome calcifie desglandes sebacees. Prog Med. 1880;8:826-8.
- Thomas RW, Perkins JA, Ruegemer JL, et al. Surgical excision of pilomatrixoma of the head and neck: a retrospective review of 26 cases. Ear Nose Throat J. 1999;78(8):541-6.
- Julian CG, Bowers PW. A clinical review of 209 pilomatricomas. J Am Acad Dermatol. 1998;39:191-5.
- Duflo S, Nicollas R, Roman S, et al. Pilomatrixoma of the head and neck in children: a study of 38 cases and a review of the literature. Arch Otolaryngol Head Neck Surg. 1998;124(11):1239-42.
- Tsoitis G, Mandinaos C, Kanitakis JC. Perforating calcifying epithelioma of Malherbe with a rapid evolution. Dermatologica. 1984;168(5):233-7.