Research Article - Journal of Primary Care and General Practice (2018) Volume 1, Issue 2
A pilot study of cholesterol management among patients in a Macau primary care setting.
In Wong*Sao Lourence Health Center, Health Bureau of Macau SAR, China
- *Corresponding Author:
- In Wong
Sao Lourence Health Centre, Health Bureau of Macau SAR, China
Tel: 00853-66861967
E-mail: michelle.wongin@gmail.com
Accepted on October 05, 2018
Abstract
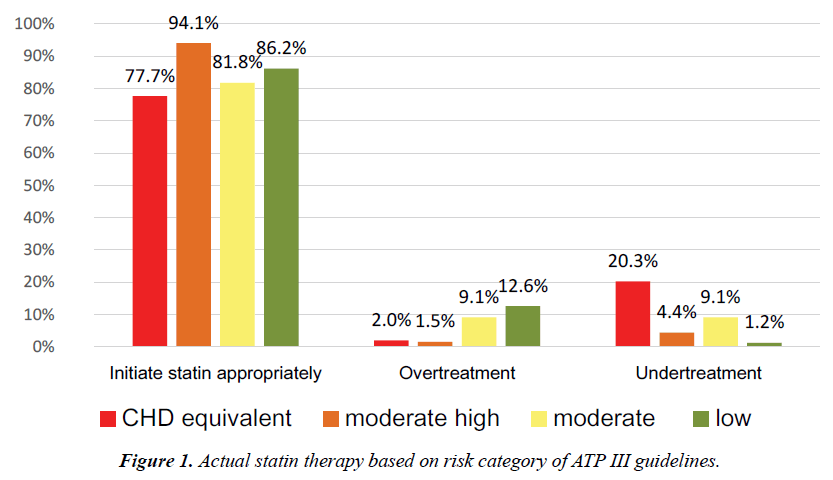
Objective: Elevated cholesterol is one of the most significant factors for cardiovascular disease. The aim of this study is to evaluate the management of dyslipidaemia in a Macau primary care setting based on the Adult Treatment Panel III guidelines. Methods: Risk estimation was based on the Framingham risk assessment and patient lipid profiles and risk factors prior to initiating statins. The results regarding the efficacy of the therapy were categorized as follows: (1) on target; (2) under treatment; (3) over treatment; and (4) managed appropriately. Results: Of the 896 patients who fulfilled the inclusion criteria, 390 (43.5%) patients were eligible for statin therapy, and 715 (79.8%) patients’ LDL-C were on target, but of the 390 patients who were eligible for statin therapy, only 214 (54.9%) patients’ LDL-C were on target. Sixty-one (20.3%) patients in the CHD equivalent group were undertreated, and the results for the other three groups were 3 (4.4%), 1 (9.1%) and 6 (1.2%) (P<0.05). Meanwhile, more patients (12.6%) were overtreated in the low-risk group, compared with other groups. Conclusions: These data suggest that nearly eighty percent of patients with dyslipidaemia in a Macau primary care setting were receiving appropriate therapy
Keywords
ATP III guidelines, cardiovascular disease prevention, cardiovascular risk, cholesterol target level, dyslipidemia.
Introduction
In Macau, cardiovascular disease (CVD) is the second leading cause of death after malignancy [1]. As well as the devastating impact CVD has on patients and their families, it also places significant pressure on our health services and economy. Dyslipidemia is one of the major risk factors for CVD [2]. There are strong evidences linking elevated low density lipoprotein cholesterol (LDL-C) to CVD and the clinical benefits of medical therapy in the treatment of dyslipidemia [2-5].
The National Cholesterol Education Program Adult Treatment Panel (ATP) III is used by most primary care physicians for cholesterol management in Macau. The ATP III guidelines recommended a “treat-to-target” strategy with specific LDL-C goals for each risk group [6]. The aim is to reach the targets using interventions that vary from lifestyle changes to pharmacological treatment [6]. For primary prevention, the guidelines consider four classes of cardiovascular risk and the LDL-C goal was set at <100 mg/dL (2.6 mmol/L) for high-risk individuals (10-year CHD risk >20%), <130 mg/dL (3.4 mmol/L) in moderate-risk patients and <160 mg/dL (4.2 mmol/L) in low-risk patients. The LDL-C goal for secondary prevention was <100 mg/dL (2.6 mmol/L), with the option to target <70 mg/dL (1.8 mmol/L) for those at highest risk of CVD [6].
In the Macau health bureau, the Framingham risk assessment [7] software has been installed in the electronic medical record system. Lipid-lowering drugs (simvastatin and gemfibrozil) in the health canter’s drug list are free of charge for all Macau residents. Other lipid-lowering drugs including rosuvastatin, atovastatin, pravastatin and fenofibrate are free of charge for patients older than 65 years of age. The government has invested so much in the prevention of cardiovascular disease, but no audit to assess the efficacy of cholesterol management in the primary care setting has been done before.
The purpose of this study was to evaluate the efficacy of cholesterol management in a Macau primary care setting by classifying the risk category and measuring the proportions of those patients who initiated statin therapy appropriately and achieved optimal cholesterol target based on the Adult Treatment Panel III guidelines [6].
Methods
This audit study was done by using computerized clinical records from 1 September 2017 to 31 December 2017. All twelve doctors who work in the Sao Lourence health center, which is one of the eight health centers in a Macau primary care setting, participated in the study. In total, 1200 patient records were systematically reviewed. Patient demographics, physical measures, lipid profile, risk factors, and concomitant medications were abstracted by reviewing computerized medical records. At the end, 896 patients fulfilled the inclusion criteria.
The inclusion criteria included the following: 1) age ≥ 21 and ≤ 75 years old, irrespective of gender; 2) the patient’s dyslipidemia is followed in the Sao Lourence health center, and there is a lipid profile record before the initiation of statin therapy; or 3) there is at least one lipid profile record within 3 years if the patient was not on statin. All the selected cases fulfilled all three criteria above.
Based on the risk assessment of ATP III guidelines [6] performed at the time of the patient starting statin therapy, the results regarding the efficacy of cholesterol management were categorized as follows: (1) on target, LDL-C lower or equal to levels of the affiliated class; (2) under treatment, patients were not on statin therapy while eligible for this; (3) overtreatment, patients were on statin even though they were not eligible for statin therapy; and (4) managed appropriately, the sum of the patients on statin whom should have been treated and the patients not on statin whom should not have been treated. The proportions of achieving optimal cholesterol target were compared between 1) between ATP III risk categories [6], and 2) between males and females. Continuous variables were expressed as the mean ± SD and categorical variables as proportions. Continuous variables in the two groups were compared using the t test; categorical variables in the different groups were compared using the Chi-square test; and where applicable, P<0.05 was considered significant. Percentages were calculated on the basis of total responses.
All the statistical analyses were carried out using SPSS version 24 (IBM Corp., Armonk, New York).
Results
Overall physician and patient cohort
A total of 896 patients were included in the study. The general characteristics of the cohort and according to sex are summarized in Table 1. The mean (± SD) age was 58.0 ± 10.1 years, and 44.4% were males. Hypertension was identified in 47.8% of patients, and 10.5% were current smokers. One-fifth (21.5%) of patients had diabetes, 10% suffered from low HDL (40 mg/ dL) and 1.6% of patients reported having a family history of premature CHD.
| Characteristic | Overall (n=896) |
Male (n=398) |
Female (n=498) |
P value |
|---|---|---|---|---|
| Age, years | 58 ± 10.1 | 58.5 ± 10.6 | 57.6 ± 9.6 | 0.158 |
| Current cigarette smoking, % | 10.5 | 19.3 | 3.4 | <0.0001 |
| Family history of premature CHD, % | 1.6 | 1.8 | 1.4 | 0.672 |
| Hypertension, %* | 47.8 | 53 | 43.6 | 0.005 |
| Low HDL cholesterol, % | 10 | 14.8 | 6.2 | <0.0001 |
| Age: male ≥45 years or female ≥55 years, % |
68 | 82.7 | 56.2 | <0.0001 |
| DM, % | 21.5 | 26.6 | 20.5 | 0.001 |
| ATP III risk categories: | --- | --- | --- | <0.0001 |
| Established CHD & CHD equivalent, % | 33.6 | 49.7 | 20.7 | |
| 2+ risk factors with 10-years risk 10-20%, % | 7.6 | 7.5 | 7.6 | |
| 2+ risk factors with 10-years risk <10%, % | 1.2 | 0.3 | 2 | |
| 0-1 risk factor | 57.6 | 42.5 | 69.7 |
*on anti-hypertensive therapy or BP ≥ 140/90 mmHg
#DM diagnosis according to ADA diagnostic criteria
ǂ10-year CHD risk calculated by Framingham risk score
Table 1: General characteristics of the cohort and according to sex
Sex differences
There were 398 men (44.4%) and 498 women in the present study. Significant sex difference is identified in this cohort (Table 1). Compared with women, men were more often smokers (19.3% versus 3.4%; P<0.0001), more had hypertension (53% versus 43.6%; P=0.005), low HDL (14.8% versus 6.2%; P<0.0001) and DM (26.6% versus 20.5%; P=0.001). No significant differences were observed in age, mean total cholesterol level and LDL-C level, but men had lower HDL levels (1.41 ± 0.42 versus 1.66 ± 0.47; P<0.0001) and higher triglyceride (TG) levels (1.86 ± 2.49 versus 1.51 ± 1.36; P=0.009) when compared with women (Table 2).
| Baseline parameter | Overall (n=896) |
Male (n=398) |
Female (n=498) |
P value |
|---|---|---|---|---|
| Total cholesterol, mmol/L | 5.69 ± 2.53 | 5.69 ± 3.6 | 5.7 ± 1.09 | 0.97 |
| HDL, mmol/L | 1.55 ± 0.47 | 1.41 ± 0.42 | 1.66 ± 0.47 | <0.0001 |
| LDL, mmol/L | 3.37 ± 1.06 | 3.35 ± 1.01 | 3.38 ± 1.1 | 0.622 |
| TG, mmol/L | 1.67 ± 1.95 | 1.86 ± 2.49 | 1.51 ± 1.36 | 0.009 |
HDL: high-density lipoprotein; LDL: low-density lipoprotein; TG: triglycerides.
The above cholesterol parameters are before starting LDL-lowering drugs or the
last lipid profile if the patient was not on pharmacological therapy.
Table 2: Cholesterol parameters for the overall cohort and according to sex
Based on ATP III guideline, more men were identified in the high-risk category (49.7% versus 20.7%; P<0.0001), and more were eligible for statin therapy (53% versus 35.9%, P<0.0001). More women were identified in the low risk category (69.7% versus 42.5%; P<0.0001) (Table 1).
Lipid parameters
Table 2 summarizes the lipid parameters for the overall cohort and according to sex. The mean (± SD) of total cholesterol level was 5.69 ± 2.53 mmol/L, HDL was 1.55 ± 0.47 mmol/L, LDL-C was 3.37 ± 1.06 mmol/L and TG was 1.67 ± 1.95 mmol/L.
Pharmacological treatment
Based on the risk assessment using the ATP III guidelines [6], there were 301 (33.6%) patients identified in the highrisk category (established CHD or 10-years CHD risk ≥ 20, diabetes mellitus); 68 (7.6%) patients in the moderate high-risk category (2+ risk factors with 10-years CHD risk 10-20%), 11 (1.2%) patients in the moderate-risk category (2+ risk factors with 10-years CHD risk <10%) and 516 (57.6%) patients in the low-risk category(0-1 risk factor). Of these 896 patients, 752 (83.9%) patients were managed appropriately, and 715 (79.8%) patients’ LDL-C was on target.
The mean LDL-C for patients who were prescribed statin was 3.47 ± 1.04, 3.34 ± 0.81, 3.24 ± 0.72, and 3.32 ± 1.10 mmol/L in the high-, moderate high-, moderate- and low-risk categories, respectively. Of these 896 patients, statin therapy was prescribed in 390 (43.9%) patients. The most commonly prescribed statin was simvastatin in 80.3% (mean dose ± SD, 18.87 ± 5.95 mg), followed by atorvastatin in 12.3% (mean dose ± SD, 20.43 ± 7.79 mg) and rosuvastatin in 7.2% (mean dose ± SD, 9.37 ± 3.87 mg). Non-statin therapies including gemfibrozil, fenofibrate and ezetimibe were used in very few patients. Combination therapy was also rarely used in this primary prevention population.
Subsequently, the appropriateness of statin prescription was assessed, based on risk level. Three hundred ninety (43.5%) patients should have been treated with statin based on the ATP III guidelines [6]. Risk assessment identified 295 individuals as high-risk who would be deemed eligible for statin therapy.
Compared with this value, the actual number of patients treated with statin was 234. Similarly, the number of patients in the moderate high-risk category who were eligible for statin therapy was 67, compared with 64 who were actually treated. In moderate-risk patients, 10 were eligible for treatment; however, the actual number treated was 9. These results suggest more under treatment (20.3%) in the high-risk category. At the same time, the analysis revealed that of the 506 patients who should not have been recommended statin therapy, 65 (12.6%) in the low-risk category, 1 (9.1%) in the moderate-risk category and 6 (2%) in the high-risk category were treated (Figure 1).
Of the 390 patients who were eligible for statin therapy, 214 (54.9%) patients met the treatment target. The comparison of proportions of achieving optimal cholesterol targets in different groups are shown in Tables 3 and 4.
| Characteristic | Overall (n=896) |
Male (n=398) |
Female (n=498) |
P value |
|---|---|---|---|---|
| Eligible for statin | 43.5 | 53 | 35.9 | <0.0001 |
| Managed appropriately*, % | 83.9 | 83.7 | 84.1 | 0.85 |
| Overtreatment, % | 8.1 | 5.5 | 10.2 | 0.01 |
| Under treatment, % | 7.9 | 10.8 | 5.6 | 0.004 |
| On target, % | 79.8 | 73.9 | 84.3 | <0.0001 |
*Managed appropriately means patients on statin whom should have been treated or the patients not on statin whom should not have been treated.
Table 3. Efficacy of cholesterol management of the overall cohort and according to sex.
| Characteristic | Overall (n=390) |
Male (n=211) |
Female (n=179) |
P value |
|---|---|---|---|---|
| Initiate statin appropriately, % | 81.8 | 79.6 | 84.4 | 0.227 |
| Under treatment, % | 18.2 | 20.4 | 15.6 | 0.227 |
| On target, % | 54.9 | 51.2 | 59.2 | 0.08 |
Table 4. Efficacy of cholesterol management of the cohort who were eligible for statin and according to sex.
Discussion
Main findings
In this first pilot study of patients with dyslipidemia in a Macau primary care setting, the objective was to evaluate whether lipid-lowering therapy was prescribed appropriately based on ATP III guidelines [6].
In Macau, lipid-lowering drugs (simvastatin and gemfibrozil) in the health center’s drug list are free of charge for all Macau residents. Other lipid-lowering drugs including rosuvastatin, atovastatin, pravastatin and fenofibrate are free of charge for patients older than 65 years of age. Under so much government investment, 71 (8.2%) patients who were eligible for statin therapy were not initiated, while 73 (14.4%) patients who likely should not have been treated were also initiated. It is notable that under treatment occurred more often in smokers and in patients with multiple risk factors. Of the patients who should have been treated, only 54.9% patients’ LDL-C was on target [6]. Failure to meet the target may be related to poor understanding of the ATP III guidelines; fear by family physicians of greater side effects related to the higher daily dosage; some drugs not being free for patients younger than 65 years; and poor compliance to treatment caused by patient concerns and awareness [8,9]. It was not the aim of the research to analyze if any of these factors were associated with poor attainment of target levels and further research will be needed to evaluate which factors influence these outcomes.
The author concluded that some physicians had not focused on intensive lipid-lowering therapy in patients at high risk, perhaps due to the limited knowledge of risk assessment of cardiovascular disease. Inappropriate or inadequate risk stratification can lead to inappropriate or inadequate treatment [10]. Consequently, it is important to develop better risk stratification tools that will be more widely and easily adopted by family physicians. Guidelines that usually to be too long and complex may contribute to clinical care gaps [11].
Although the ATP III guideline has been in place for nearly 15 years, it remains the most widely used guideline by Macau family physicians, and the Framingham risk assessment software is already set up in the electronic medical record system of the Macau health bureau. In 2013, the AHA/ACC introduced a new risk calculator to the public domain and challenged the notion of treat-to-targets strategy [12,13]. The impact of conflicting guidelines will potentially make it even more difficult for family physicians to stratify their patients’ risk appropriately. Further research will be needed to evaluate which guideline is most appropriate to use in the Macau primary care setting.
Strengths and limitations of the study
In the management of dyslipidemia, patient preferences, comorbidities, concomitant drugs, potential side effects, family history and non-incorporated risk factors all play a role. One of the limitations of my research was the inability to determine how much these factors influenced physician decision making. Another limitation was only a small number of family physicians and only one health center in Macau primary care setting took part in the research. The selection bias cannot be excluded in that the participating physicians likely had more or less of an ability in lipid management and, thus, may not be fully representative of the broader family physician population in Macau. The strengths of this study are that all identification cases routinely used electronic medical record and the unique perspective of a Macau primary care setting.
Conclusion
These data suggest nearly eighty percent of patients with dyslipidaemia in a Macau primary care setting are receiving appropriate management, but cholesterol management is not always optimal in all risk categories. Of the patients who are eligible for statin therapy, nearly half did not meet the treatment goal. An intervention comprising feedback from the audit and staff training in translating cholesterol guidelines into primary care practice should be initiated in order to optimize the cholesterol management in the Macau primary care setting.
Acknowledgements
I acknowledge the support provided by the director of the Sao Lourence Health Center and the GPs who participated in my research study.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure Statement
The authors declare that they have no conflict of interest.
Ethical Approval
The patients' identities were protected, and no individual patients could be identified from the data. Ethical approval for the study was obtained from the Medical Ethical Committee of Centro Hospitalar Conde de Sao Januario. The patients and doctors involved were not at risk of harm because this study was only an audit of patients with dyslipidaemia.
References
- de Saúde S, da Região G. Administrativa especial de Macau. Boletim estatístico [Internet]. 2016.
- Wilson PWF, D'Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837-47.
- Stamler J, Wentworth D, Neaton JD, et al. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356 222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986; 256:2823-8.
- Lipid Research Clinics Program. The Lipid Research Clinics Coronary Primary Prevention Trial results. II: The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984; 251:365-74.
- Pekkanen J, Linn S, Heiss G, et al. Ten-year mortality from cardiovascular disease in relation to cholesterol level among men with and without preexisting cardiovascular disease. N Engl J Med. 1990; 322:1700-7.
- National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health. Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. NIH Publication No. 02-5215. Bethesda, MD: National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, 2002.
- D'Agostino RB Sr1, Vasan RS, Pencina MJ. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008; 117(6):743-53.
- Raithatha N, Smith RD. Paying for statins. BMJ 2004; 328: 400-402.
- Cacoub P, Tocque-Le Gousse E, Fabry C, et al. Application in general practice of treatment guidelines for patients with dyslipidaemia: the RESPECT study. Archives of Cardiovascular Diseases 2008; 101: 715-721.
- Erhardt LR, Hobbs FD. A global survey of physicians’ perceptions on cholesterol management: the From The Heart study. International Journal of Clinical Practice 2007; 61: 1078-1085.
- Institute of Medicine (U.S.) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. Washington, DC: National Academics Press; 2011.
- Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2889-934.
- Anderson TJ, Gregoire J, Hegele RA, et al. Are the ACC/AHA Guidelines on the treatment of blood cholesterol a game changer? A perspective from the Canadian Cardiovascular Society dyslipidemia panel. Can J Cardiol. 2014; 30:377-80.