Research Article - Current Pediatric Research (2023) Volume 27, Issue 6
A pilot cross-sectional study for dorsiflexion hinged ankle-foot orthosis on spatiotemporal gait parameters in children with spastic diplegic cerebral palsy.
Kyeongbong Lee1, GyuChang Lee2*
1Department of Physical Therapy, Kangwon National University, Samcheok, Republic of Korea
2Outreach Physical and Occupational Therapy and Speech Rehabilitation PLLC, New York, USA
- Corresponding Author:
- GyuChang Lee,
GyuChang Lee. PT. Ph.D. Outreach Physical, Occupational, and Speech Therapy. 1110 2nd Ave # 302, New York, NY 10022 United States
E-mail: leegc76@hanmail.net
Received: 26 May, 2023, Manuscript No. AAJCP-23-99430; Editor assigned: 29 May, 2023, Pre QC No. AAJCP-23-99430(PQ); Reviewed: 12 June, 2023, QC No. AAJCP-23-99430; Revised: 19 June, 2023, Manuscript No. AAJCP-23-99430(R); Published: 29 June, 2023, DOI:10.35841/0971-9032.27.06.1911-1918.
Abstract
Background: Ankle Foot Orthosis (AFO) is one of the most prescribed orthoses for children with spastic diplegic Cerebral Palsy (CP), and there are numerous types for various purposes. The results of previous studies regarding the effects and positive effects of AFO on CP gait are unclear. The purpose of this study is to compare the gait parameters by the angle change of the AFO to investigate the effect of Dorsiflexion-Hinged AFO (DHAFO).
Methods: 10 subjects with spastic diplegic CP participated in this study. The spatial (cadence, step length, and stride length) and temporal (gait velocity, single- and double-limbs support time) gait parameters were obtained and compared by subjects with flexible equinus with bare feet, AFO, and DHAFO. This study, a cross-sectional study, measured a total of three times at two-day intervals and derived the average value.
Results: Spatial and temporal parameters measured under the three conditions showed significant differences (F=6.469~24.914, P=0.000~0.008, partial eta square=0.621~0.887). The gait with DHAFO showed significant differences in cadence and stride length compared to bare feet and AFO (P<0.05) in spatial parameters. In addition, DHAFO gait demonstrated significant differences in all temporal parameters compared to bare feet and AFO (P<0.05).
Conclusion: In this study, it was found that DHAFO was different from gait with bare feet and AFO on spatiotemporal parameters in children with spastic diplegic CP. Although the factors affecting gait ability are very diverse, DHAFO is considered to be one of the orthoses that can improve ambulatory function in CP with equinus.
Keywords
Ankle foot orthosis, Dorsiflexion, Gait, Spasticity, Diplegia, Cerebral palsy.
Abbreviations
CP: Cerebral Palsy; AFO: Ankle Foot Orthosis; DHAFO: 10° Dorsiflexion Hinged; GMFCS: Gross Motor Function Classification System.
Introduction
Cerebral Palsy (CP) is a non-progressive disorder caused by brain defects or lesions of the brain that occur before or during birth or within 2 years of birth [1]. This disorder is caused by damage to the brain and is usually accompanied by neurological impairments, resulting in permanent problems with limb strength and control [2]. Due to neurological impairment, neuromuscular control ability may be reduced and musculoskeletal disorders may occur. There is no single intervention method to treat CP, but functional outcomes can be improved through early therapeutic intervention [3].
CP can be categorized into spasticity, dystonia, choreoathetosis, or ataxia according to abnormal muscle tone, involuntary movement, and postural deformation, the simultaneous activity of agonist and antagonist muscles, muscle weakness, and abnormal coordination [4]. The spasticity type is known as the most common type at 83%-88%, and dyskinetic and ataxic CP (8%-12% and 3%-4%, relatively) show relatively low rates. Children with spastic CP experience various difficulties in gait due to decreased selective motor control, weakness, and contracture [5]. Thus, their quality of life is inevitably reduced due to the decline in gait ability; the main purpose of most interventions for CP is to increase participation in daily life with the improvement of independent gait.
Spastic diplegic CP is characterized by reduced motor control in the lower limbs, especially impaired motor control of the distal lower extremities [6]. Muscle strength, gross motor coordination, and balance are all imperative for independent gait in children with CP. However, there is no consensus on the most ideal therapeutic approach as growth progresses [7]. Diplegic CP refers to a case in which the function of the lower extremities is relatively lower than that of the upper extremities; more than 50% of subjects diagnosed with spastic CP have diplegia [8]. Since weakness and tightness due to spasticity can usually occur in the hip joint and pelvis as well, an overall decrease in gait ability is observed [9]. The most common pattern seen in spastic diplegic CP is the jump gait, accompanied by calf spasticity as well as hamstrings and hip flexors [10]. In addition, secondary complications such as muscle contracture, skeletal deformities, hip dislocation, and scoliosis may occur due to an imbalance between these muscles [11]. In most cases of diplegic CP, independent ambulation may be possible, but appropriate assistive devices can be needed because various problems in gait may occur due to the dysfunction of these muscles.
Even though there is no strong evidence for their effectiveness, orthoses are broadly used in the intervention of children with CP, Ankle-Foot Orthosis (AFO) is the most commonly used [12]. AFO is utilized to improve gait function and alignment of the body, and it increases the gait speed and reduces the energy consumption of children with CP [13]. In addition, AFO used to improve range of motion may be more effective for CP children with reduced dorsiflexion [14]. Solid AFO, dynamic AFO, floor reaction orthosis, posterior leaf spring, and hinged AFO are the main orthoses used in CP rehabilitation, and all may improve gait function through a mechanism that reduces excessive plantar flexion [15]. Another systematic review reported that AFO is advantageous for improving the gait speed of unilateral CP, and dynamic AFO is most suitable for improving ankle kinematics of bilateral CP [16]. As such, various results on AFO have been reported, which is commonly used in CP rehabilitation, but studies comparing changes in gait-related variables of children with CP according to the angle of AFO are deficient.
Since AFO is a common and easily used orthosis to improve the independent gait ability of children with cerebral palsy, this study aimed to find out the spatiotemporal gait parameters of children with spastic diplegic cerebral palsy may change according to the angle of AFO. We hypothesized that there would be differences in gait-related variables when a constant change was applied to the plantar flexed ankle joint, which is one of the characteristics of children with spastic diplegic cerebral palsy.
Materials and Methods
Study design
This is a pilot cross-sectional study for AFO on spatiotemporal gait parameters in children with spastic diplegic cerebral palsy. To find out whether there is a difference in the gait of children with spastic diplegic cerebral palsy depending on the angle of AFO, spatiotemporal gait parameters were measured and compared in bare feet, HAFO, and wearing a 10° dorsiflexion hinged AFO (DHAFO).
Participants
The subjects of this study were children with spastic diplegic cerebral palsy, the participants were recruited and the details of this study were posted for one month to employee volunteers in the S Rehabilitation Research Institute and S Rehabilitation Center located in the Republic of Korea. The inclusion criteria were as follows: 1) Who have been diagnosed with spastic diplegic CP by a doctor; 2) Aged between 4 and 15 years; 3) Had flexible equinus; 4) Who were classified as Gross Motor Function Classification System (GMFCS) I or II; 5) Who could conduct independent gait; 6) No use of assistive devices; 7) Who has dynamic equines deformity; 8) Who have worn AFO for more than 6 months and received gait related rehabilitation intervention.
Exclusion criteria were as follows: 1) Use of medications for neuromuscular control or that provoke drowsiness; 2) Who have epilepsy or are taking related drugs; 3) With history of surgery within the last 6 months; and 4) Severe cognitive or visual impairments. A total of 13 participants were recruited, and 3 dropped out due to personal reasons of their caregivers. The subjects who participated in the experiment were 7 males and 3 females, and their age was 9.7 ± 3.2 years. The general characteristics of the subjects through brief interviews are described in Table 1. This study was conducted with the approval of the Institutional Review Board of Kyungnam University (approval number: 1040460-A-2018-040, approval date: August 20, 2018).
| Variables | N (%) |
|---|---|
| GMFCS level (Ⅰ/Ⅱ) | 4 (40%)/6 (60%) |
| Gender (male/female) | 7 (70%)/3 (30%) |
| M (SD) | |
| Age (years) | 9.725 (3.218) |
| Height (cm) | 127.482 (10.437) |
| Weight (kg) | 29.143 (8.238) |
| Disease duration (month) | 94.821 (13.019) |
| Note: M (SD): Mean (Standard Deviation); GMFCS: Gross Motor Function Measurement Level. | |
Table 1. General information of participants.
Gross motor function classification system
The GMFCS is one of the evaluation tools that can effectively explain the subject's mobility level to the family of children with CP by medical professionals, and generalizing the level of the current subject can help set the goal of the intervention. The GMFCS consists of a 5-level classification system; it describes the subject's gross motor function that emphasizes self-initiated movement in sitting, walking, and wheeled mobility [17]. It was set based on the GMFCS evaluated by the physical therapists in charge of the subjects who volunteered to participate in the experiment. The inter-rater reliability of the GMFCS was reported to be 0.84 and the GMFCS level was moderately correlated with other gross motor tests [18].
Spatiotemporal gait parameters
The spatiotemporal gait parameters were measured by using the GAITRite® electronic walkway (CIR Industries, Clifton, NJ, USA) portable gait analysis device at 5.186 m at the speed selected by the participant. This walkway has a built-in pressure sensor in the horizontal direction, which digitizes the pressure caused by the feet position and weight of the subject while walking. The children with CP walk on the walkway, and the delivered pressure and time are transmitted to the computer through the sensor. The data obtained through the results of each step are computerized into spatial (distance) and temporal (time) parameters for assessing gait. This device has an excellent level of agreement with Intra-Class Correlation Coefficients (ICCs) between 0.92 and 0.99 for walking speed, cadence, step length, and step time variables [19], and test– retest reliability [20].
Procedure
Among the volunteers for this study, spatiotemporal gait parameters were measured for children with CP who corresponded to GMFCS I and II. To match the purpose of this study, subjects were selected who angle of the ankle joint could changes according to the angle set in the AFO during gait. After sufficiently explaining the procedure of this study to the subjects and their caregivers, the physical therapist in charge performed a demonstration to reduce the awkwardness of the electronic walkway.
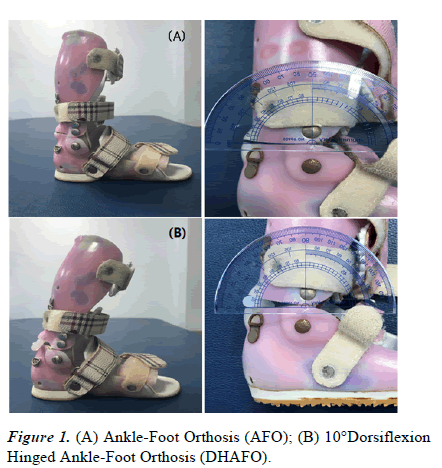
With the supervision of research assistants and caregivers, the results of spatiotemporal gait parameters were measured with bare feet, AFO (Figure 1A), and DHAFO (Figure 1B). The AFO used in this study was prepared according to the characteristics of each participant after being prescribed by the physician in charge. The DHAFO were made of a 4.8 mm thick polyester material most used in clinics. It is made to wrap from the bottom of the toe to the inner edge of the foot and climb up to the back of the calf to connect to the 2.5 cm to 5 cm below the knees. It fixed 7 mm glue to the hinge at the back of the AFO by using a 7 mm glue stick to induce 10° dorsiflexion.
Measurement of each participant's spatiotemporal gait parameters was performed with bare feet, AFO, and DHAFO in random order to minimize the bias for the sequence. Because the study was conducted with children, measurements were taken once a day, and a 15-minute break was provided between trials. The evaluations were taken three times at twoday intervals, and the results of this study were obtained as the average value of a total of three measurements. Cadence, step length, and stride length were measured as spatial gait parameters, and gait velocity, single-leg support time, and double-leg support time were evaluated as temporal gait parameters. Since this study was conducted on diplegic CP, variables in both lower limbs were obtained.
Statistical analysis
The number of measurements was 3, the α-value was set to 0.05, and the power (1-β error probability) value was set to 0.8 (G*power 3.1.9.7, Kiel University, Germany) [21]. Cohen’s effect size was set to 0.25, 28 subjects were needed to complete this study based on these conditions.
The normal distribution was identified by the Kolmogorov- Smirnov test for the spatiotemporal gait parameters with bare feet; all variables satisfied the normal distribution. Repeated measures analysis of variance was performed to find out the difference within the subjects in spatiotemporal gait parameters with bare feet, AFO, and DHAFO.
The spatiotemporal gait parameters measured on both lower limbs for bare feet, AFO, and DHAFO satisfied Mauchly's test of sphericity (p>0.05), so the sphericity assumption was met out data. The results of the present study didn’t need any correction such as Greenhouse-Geisser or Huynh-Feldt, and post hoc comparisons were performed using the Bonferroni correction. Statistical analysis was performed using the Statistical Package for the Social Sciences version 23.0 software (IBM corp., Armonk, NY), results were considered significant with a pvalue of p<0.05.
Results
The results of 10 subjects who performed all the procedures of this study were analyzed. As a result of repeated measurements on spatiotemporal gait parameters performed with bare feet, AFO, and DHAFO (Table 2), there were significant differences in spatial and temporal parameters (F=6.469~24.914, P=0.000~0.008, partial eta square=0.621~0.821; F=11.046~39.761, P=0.000~0.001, partial eta square=0.683~0.887, respectively).
| Parameters | Type III SS | Df | Mean square | F | P-value | Partial eta square | |
|---|---|---|---|---|---|---|---|
| Spatial parameters | |||||||
| Cadence (cm) | 3214.881 | 2 | 1607.44 | 24.914 | P=0.000 | 0.821 | |
| Step length (cm) | Lt | 152.877 | 2 | 76.439 | 10.27 | P=0.001 | 0.642 |
| Rt | 246.093 | 2 | 123.046 | 6.469 | P=0.008 | 0.621 | |
| Stride length (cm) | Lt | 862.158 | 2 | 431.079 | 12.624 | P=0.000 | 0.745 |
| Rt | 841.904 | 2 | 420.952 | 12.112 | P=0.000 | 0.735 | |
| Temporal parameters | |||||||
| Gait velocity (cm/sec) | 3391.089 | 2 | 1695.544 | 39.761 | P=0.000 | 0.887 | |
| Single-limb support time (sec) | Lt | 0.04 | 2 | 0.02 | 11.046 | P=0.001 | 0.752 |
| Rt | 0.037 | 2 | 0.018 | 12.031 | P=0.000 | 0.683 | |
| Double-limb support time (sec) | Lt | 0.115 | 2 | 0.058 | 11.096 | P=0.001 | 0.857 |
| Rt | 0.134 | 2 | 0.067 | 11.634 | P=0.001 | 0.836 | |
| Note: SS: Sum of Square; Df: Degree of Freedom; AFO: Hinged Ankle Foot Orthosis; DHAFO: 10° Dorsiflexion Hinged Ankle Foot Orthosis; L/E: Lower Extremity. | |||||||
Table 2. The summary of one-way repeated measure ANOVA testing for the differences of bare feet, AFO and DHAFO in spatiotemporal gait parameters. (N=10).
Table 3 describes summary statistics to find out the difference in the spatiotemporal gait parameters between each of the three gait conditions. Spatial parameters showed no difference between bare feet and wearing AFO. However, with bare feet and DHAFO, there were significant differences were found in spatial and temporal parameters (P<0.05). In addition, significant differences were revealed in cadence and stride length in comparison to AFO and DHAFO. In temporal parameters, comparing single support time and double support time, significant differences were found between bare feet and AFO (P<0.05). In comparison between bare feet and DHAFO, significant differences were found in all temporal gait parameters (P<0.05), and comparison between AFO and DHAFO also showed the same results (P<0.05).
| Parameters | Bare feet | AFO | DHAFO | P-value | |
|---|---|---|---|---|---|
| Spatial parameters | |||||
| Cadence (cm) | 89.17 ± 18.81 | 97.52 ± 12.05 | 114.08 ± 15.95bc | P=0.000 | |
| Step length (cm) | Lt | 32.79 ± 4.56 | 34.75 ± 4.98 | 38.25 ± 4.51b | P=0.001 |
| Rt | 32.06 ± 3.60 | 32.64 ± 7.68 | 38.40 ± 7.95b | P=0.008 | |
| Stride length (cm) | Lt | 64.02 ± 7.93 | 67.94 ± 11.88 | 76.99 ± 10.41bc | P=0.000 |
| Rt | 64.25 ± 7.25 | 67.31 ± 11.68 | 76.41 ± 10.43bc | P=0.000 | |
| Temporal parameters | |||||
| Gait velocity (cm/sec) | 48.44 ± 12.28 | 55.05 ± 12.99 | 73.56 ± 17.99bc | P=0.000 | |
| Single-limb support time (sec) | Lt | 0.45 ± 0.07 | 0.41 ± 0.05a | 0.36 ± 0.02bc | P=0.001 |
| Rt | 0.45 ± 0.07 | 0.41 ± 0.04a | 0.36 ± 0.02bc | P=0.000 | |
| Double-limb support time (sec) | Lt | 0.47 ± 0.19 | 0.41 ± 0.17a | 0.32 ± 0.15bc | P=0.001 |
| Rt | 0.47 ± 0.21 | 0.41 ± 0.17a | 0.32 ± 0.14bc | P=0.001 | |
| Note: The values are expressed as mean ± standard deviation. Superscript ‘a’ means aSignificant difference between bare feet and AFO; bMeans a significant difference between bare feet and DHAFO and; cMeans a significant difference between AFO and DHAFO. Abbreviations: Hinged Ankle Foot Orthosis (HAFO, AFO); 10° dorsiflexion hinged ankle foot orthosis (DHAFO). |
|||||
Table 3. Multiple comparisons of spatiotemporal gait parameters with bare feet, AFO and DHAFO (N=10).
Discussion
This is a pilot cross-sectional study to find out the difference in spatiotemporal gait parameters according to the condition of AFO in children with spastic diplegic CP. The present study was conducted in CP children with GMFCS I and II, the AFOs were found to be different even though it may be considered a spontaneous result. In addition, a meaningful difference was found in spatiotemporal gait parameters with DHAFO compared to AFO, which maintains the neutral position of the ankle.
AFO provides internal and external stability of the feet and ankles in standing or walking [22]. It is frequently used to improve gait ability, such as gait velocity and stride length. Spastic diplegic CP has impaired control of bilateral lower extremities; AFO with the ankle joint fixed at 90° is commonly utilized in clinical settings due to insufficient dorsiflexion of the ankle. Since spastic diplegic CP causes greater muscle dysfunction in the distal lower extremity [23], AFO is one of the most commonly used orthoses [24]. Among 2200 subjects, 51% were using AFO, 10% improved physical function, and 11% reported an improvement in range of motion and a 30% improvement in both. In addition, functional goals were achieved in 73% of CP children using AFO, and the range of ankle dorsiflexion was maintained or improved by 70%.
AFO increases the stride length and decreases abnormal plantarflexion angle at initial contact, midstance, and terminal stance [25]. And it raises ankle dorsiflexion at the terminal stance and increases ankle movement during pre-swing. In addition, the gait velocity and stride length can be improved with community-prescribed AFO compared to bare feet; however, there was no difference in cadence [26]. Another study reported that wearing a hinged AFO took less energy for walking and increased gait velocity than bare feet, so it made more efficient gait function. In a study, on the effect of AFO on gait indices in diplegic CP, reported that temporal and kinematic parameters showed meaningful improvement [27]. More than 80% of children with CP are prescribed and using AFO and it is effective for step length and gait velocity, but not all gait indices were improved [28].
This study was also similar to the results of previous studies; there was no difference in spatial parameters when comparing bare feet with AFO. Temporal parameters were shorter when wearing the AFO except for gait velocity. This may be considered a spontaneous result because the factors influencing gait parameters in children with spastic diplegic CP include not only the ankle joint but also structural impairments of the other joints of the lower extremities. Gait does not involve the use of only one joint, and when there is impairment in both lower extremities; differences in all gait-related variables may not be found only with AFO. However, compared to bare feet, the shorter time of single- and double-limb support in gait with AFO is considered the swing phase of the contralateral leg could be performed easier because AFO increased the stability of the feet and ankle.
The AFO is the most commonly prescribed orthosis for spastic diplegic CP for various reasons, though, it has various limitations due to reducing the push-off power during the gait cycle, hip joint compensation, and higher dose of energy cost occurs [29]. Proper cooperation of joints and muscles of the lower extremities is required to perform the gait cycle consisting of stance and swing phase, and dorsiflexion of 10°-20° is required especially in the ankle joint [30,31]. The dorsiflexion angle of AFO should be allowed at least 10° to achieve functional gait [32]. However, these previous studies compared bare feet to wearing AFO, or compared gait when wearing various types of AFO. Thus, this study hypothesized that the spatiotemporal gait parameters may be different compared to AFO with DHAFO.
A DHAFO may increase stable weight support by aligning the rear foot and the mid-foot during the stance phase [33]. In addition, DHAFO could further improve foot clearance in the swing phase, resulting in the advance of other gait parameters including step length and stride length. Regardless of the type of AFO, it has the effect of reducing pathological plantar flexion in diplegic CP with impairment of gait pattern [34]. In children with spastic diplegic CP, the ground reaction force is increased in push-off with AFO, and AFO with dorsiflexion of 5° or more can ideally induce the length of calf muscles and progress plantar flexion moment close to the normal value. Ankle dorsiflexion is necessary for terminal stance and can affect the kinematics of the knee joint.
Knee joint kinematics and kinetics in the sagittal and frontal planes were affected by reduced ankle dorsiflexion during the terminal stance of gait. Differences were observed with restriction in the ankle dorsiflexion range of approximately 8° [35]. The results of this study were similar to the previous studies, and spatiotemporal parameters were more advanced in DHAFO than in bare feet and AFO. For comparison under the same conditions, the evaluation was performed on subjects with diplegic equinus, and the parameters were more prominent in DHAFO to compensate for insufficient dorsiflexion in the ankle. It is thought that DHAFO more effectively supplemented the plantar flexion moment in the terminal stance than AFO, and the foot clearance in the swing phase which were deficient due to ankle equinus.
Although spastic diplegic CP is not possible to walk close to normal gait only with the ankle approach, it was found that DHAFO might have a positive effect on gait parameters compared to AFO. AFOs induce small improvements in gait speed and moderate evidence that AFOs have a small to moderate effect on gross motor function [16]. In CP with equinus, in particular, DHAFO had a strong level of evidence for important changes in the kinematics of both distal limbs. Thus, DHAFO made higher values of gait velocity by increasing the dorsiflexion angle during the initial contact and the swing phase in the gait cycle. In patients who needed plantar flexion control due to drop foot, the deviation was decreased by the initial contact in the gait cycle while wearing AFO with dorsiflexion assist [36]. Although it may be difficult to conclude that the positive factors that AFO affects gait in children with spastic diplegic CP are clear, it is considered important to apply a customized orthosis for each subject's neuromuscular condition.
The present study has several limitations requiring future research. First, the number of subjects who participated in this study was too small; the results of this study cannot be generalized in children with spastic diplegic CP [37]. However, it was difficult to efficiently recruit applicants due to the pandemic situation, and this research is a pilot cross-sectional study to investigate the long-term effect of DHAFO. Second, although only ankle orthoses are not utilized to improve gait in children with CP, only gait parameters by bare feet, AFO, and DHAFO were evaluated. Gait can be performed through coordination of not only the ankle but also the knee, hip, and trunk. However, in the case of spastic diplegic CP, AFO is the most common and easily applied orthosis, thus this study compared the immediate difference in gait parameters due to a simple angle change of AFO [38].
Third, it is necessary to consider the bias caused by the mental and physical conditions of the participants because children with CP were the subjects although the results were derived through three sessions of measurement within one week. Lastly, only children with spastic diplegic CP belonging to GMFCS I and II were included. Since these subjects are at a level at which independent ambulation is possible, their gait level may be improved with any orthosis. However, this study is a study to find out whether DHAFO has different results of the parameters from bare feet and AFO, subjects with flexible ankle equinus that DHAFO can adhere to the foot and ankle were selected [39].
Conclusion
AFO is the most commonly used orthosis to improve gait ability, the findings show that there was a meaningful difference in the spatiotemporal gait parameters of DHAFO compared to bare feet and AFO applied to children with spastic diplegic CP. Although the factors that affect gait are very diverse, spastic diplegic CP with ankle equinus showed more improved results in DHAFO with dorsiflexion added from a cross-sectional point of view. In future studies, it is necessary to investigate the effect of training using DHAFO on gait parameters and functional ambulation in children with spastic diplegic CP.
Ethics Approval and Consent to Participate
After the study received approval from the institutional review board of Kyungnam University (approval number: 1040460- A-2018-040, approval date: August 20, 2018), all subjects and their legal representatives listened to an explanation of the study purpose and procedures before voluntarily signing a children’s agreement and a legal representative’s agreement.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not applicable
Acknowledgements
Not applicable
References
- Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 2005; 47(8): 571–6.
- Damiano DL, Alter KE, Chambers H. New clinical and research trends in lower extremity management for ambulatory children with cerebral palsy. Phys Med Rehabil Clin N Am 2009; 20(3): 469–91.
- Malhotra A. Editorial: Early detection and early intervention strategies for cerebral palsy in low and high resource settings. Brain Sci 2022; 12(8): 960.
- Bekteshi S, Monbaliu E, McIntyre S, et al. Towards functional improvement of motor disorders associated with cerebral palsy. Lancet Neurol 2023; 22(3): 229–43.
- Zhou J, Butler EE, Rose J. Neurologic correlates of gait abnormalities in cerebral palsy: Implications for treatment. Front Hum Neurosci 2017; 11: 103.
- Fowler EG, Staudt LA, Greenberg MB. Lower-extremity selective voluntary motor control in patients with spastic cerebral palsy: increased distal motor impairment. Dev Med Child Neurol 2010; 52(3): 264–9.
- Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: State of the evidence. Dev Med Child Neurol 2013; 55(10): 885–910.
- Graham HK, Rosenbaum P, Paneth N, et al. Cerebral palsy. Nat Rev Dis Primers 2016; 2: 15082.
- Huntsman R, Lemire E, Norton J, et al. The differential diagnosis of spastic diplegia. Arch Dis Child 2015; 100(5): 500–4.
- Rodda J, Graham HK. Classification of gait patterns in spastic hemiplegia and spastic diplegia: a basis for a management algorithm. Eur J Neurol 2001; 8 Suppl 5: 98–108.
- Morrell DS, Pearson JM, Sauser DD. Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics 2002; 22(2): 257–68.
- Morris C, Bowers R, Ross K, et al. Orthotic management of cerebral palsy: Recommendations from a consensus conference. NeuroRehabilitation 2011; 28(1): 37–46.
- Brehm MA, Harlaar J, Schwartz M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J Rehabil Med 2008; 40(7): 529–34.
- Wingstrand M, Hägglund G, Rodby-Bousquet E. Ankle-foot orthoses in children with cerebral palsy: A cross sectional population based study of 2200 children. BMC Musculoskeletal Disord 2014; 15: 327.
- Aboutorabi A, Arazpour M, Ahmadi Bani M, et al. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann Phys Rehabil Med 2017; 60(6): 393–402.
- Lintanf M, Bourseul JS, Houx L, et al. Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: A systematic review and meta-analysis. Clin Rehabil 2018; 32(9): 1175–88.
- Palisano RJ, Rosenbaum P, Bartlett D, et al. Content validity of the expanded and revised gross motor function classification system. Dev Med Child Neurol 2008; 50(10): 744–50.
- Bodkin AW, Robinson C, Perales FP. Reliability and validity of the gross motor function classification system for cerebral palsy. Pediatr Phys Ther 2003; 15(4): 247–52.
- Webster KE, Wittwer JE, Feller JA. Validity of the GAITRite walkway system for the measurement of averaged and individual step parameters of gait. Gait Posture 2005; 22(4): 317–21.
- van Uden CJT, Besser MP. Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite). BMC Musculoskelet Disord 2004; 5: 13.
- Faul F, Erdfelder E, Lang AG, et al. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39(2): 175–91.
- Betancourt JP, Eleeh P, Stark S, et al. Impact of ankle-foot orthosis on gait efficiency in ambulatory children with cerebral palsy: A systematic review and meta-analysis. Am J Phys Med Rehabil 2019; 98(9): 759–70.
- Wakeling J, Delaney R, Dudkiewicz I. A method for quantifying dynamic muscle dysfunction in children and young adults with cerebral palsy. Gait Posture 2007; 25(4): 580–9.
- Meyns P, Kerkum YL, Brehm MA, et al. Ankle foot orthoses in cerebral palsy: Effects of ankle stiffness on trunk kinematics, gait stability and energy cost of walking. Eur J Paediatr Neurol 2020; 26: 68–74.
- Radtka SA, Skinner SR, Elise Johanson M. A comparison of gait with solid and hinged ankle-foot orthoses in children with spastic diplegic cerebral palsy. Gait Posture 2005; 21(3): 303–10.
- Hayek S, Hemo Y, Chamis S, et al. The effect of community-prescribed ankle–foot orthoses on gait parameters in children with spastic cerebral palsy. J Child Orthop 2007; 1(6): 325–32.
- Danino B, Erel S, Kfir M, et al. Are gait indices sensitive enough to reflect the effect of ankle foot orthosis on gait impairment in cerebral palsy diplegic patients? J Pediatr Orthop 2016; 36(3): 294.
- Everaert L, Papageorgiou E, Van Campenhout A, et al. The influence of ankle-foot orthoses on gait pathology in children with cerebral palsy: A retrospective study. Gait Posture 2023; 100: 149–56.
- Yvette Kerkum L, Annemieke Buizer I, Josien C van den N, et al. The effects of varying ankle foot orthosis stiffness on gait in children with spastic cerebral palsy who walk with excessive knee flexion. PloS One 2015; 10(11): e0142878.
- Grimston SK, Nigg BM, Hanley DA, et al. Differences in ankle joint complex range of motion as a function of age. Foot Ankle 1993; 14(4): 215–22.
- Stauffer RN, Chao EY, Brewster RC. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat Res 1977; (127): 189–96.
- Skrotzky K. Gait analysis in cerebral palsied and nonhandicapped children. Arch Phys Med Rehabil 1983; 64(7): 291–5.
- Zettel JL, McIlroy WE, Maki BE. Environmental constraints on foot trajectory reveal the capacity for modulation of anticipatory postural adjustments during rapid triggered stepping reactions. Exp Brain Res 2002; 146(1): 38–47.
- Lam WK, Leong JCY, Li YH, et al. Biomechanical and electromyographic evaluation of ankle foot orthosis and dynamic ankle foot orthosis in spastic cerebral palsy. Gait Posture 2005; 22(3): 189–97.
- Ota S, Ueda M, Aimoto K, et al. Acute influence of restricted ankle dorsiflexion angle on knee joint mechanics during gait. The Knee 2014; 21(3): 669–75.
- Khan MK, Bibi U, Shah W. Comparing the effect of leaf spring and swedish afo in patient with drop foot deformity (PERONEAL nerve injury). J Prosthet Orthot Sci Technol 2023; 2(1): 11–4.
- Kim CS, Young PS. Effects of an ankle foot orthosis with ankle angles on balance performance in healthy adults. J Ergon Soc Korea 2011; 30(2): 291–6.
- Wright E, DiBello SA. Principles of ankle-foot orthosis prescription in ambulatory bilateral cerebral palsy. Phys Med Rehabil Clin N Am 2020; 31(1): 69–89.
- Nazha HM, Szávai S, Darwich MA, et al. Passive articulated and non-articulated ankle–foot orthoses for gait rehabilitation: A narrative review. Healthcare (Basel) 2023; 11(7): 947.