Research Article - Biomedical Research (2017) Volume 28, Issue 6
A morphometric evaluation of the humeral component in shoulder arthroplasty
Cihan Iyem1, Sancar Serbest2*, Mikail Inal3, Veysel Burulday3, Ahmet Kaya3, Turgut Kultur4 and Ugur Tiftikci21Department of Anatomy, Faculty of Medicine, University of Kirikkale, Turkey
2Department of Orthopaedics and Traumatology, Faculty of Medicine, University of Kirikkale, Turkey
3Department of Radiology, Faculty of Medicine, University of Kirikkale, Turkey
4Department of Physical Medicine and Rehabilitation, Faculty of Medicine, University of Kirikkale, Turkey
- *Corresponding Author:
- Sancar Serbest
Department of Orthopaedics and Traumatology, Faculty of Medicine
Kirikkale University, Turkey
Accepted date: November 8, 2016
Abstract
Purpose: Aim of the study is to make a clinical evaluation of parameters used in prosthesis design for the humeral component applied in arthroplasty of the proximal upper extremity.
Methods: In our study the plain shoulder radiographs were used of 195 (101 male, 94 female) patients aged 18-65 years (mean age, 38.8 ± 11.5 years; males 35.4 ± 11.6 years, females 42.5 ± 10.2) with soft tissue trauma, but no degenerative or structural disorder in the shoulder joint (fracture, tumour, osteoarthritis etc.). Measurements were made on the radiograph of Head Height (HH), Frontal Base Diameter of the Head (FBD), 3 points at 3 cm intervals from proximal to distal of the medullar canal at surgical neck Endosteal Diameter (ED1, ED2 and ED3 respectively), Neck-Shaft Angle (NSA) and Head- Neck Angle (HNA).
Results: According to the results, in the comparison of Groups I and III except the mean values of HH and ED1 in other parameters, no statistically significant difference was determined. In the comparison of Groups II and IV except the mean values of FBD and ED1 in other parameters no statistically significant difference was determined.
Conclusions: In conclusion, the success of shoulder arthroplasty is explained well by the anatomic structure and proximal humerus morphometric parameters examined in this study. In prosthesis design, the differences in age and populations should be taken.
Keywords
Prosthesis, Humeral head, Arthroplasty.
Introduction
In current shoulder arthroplasty applied for traumatic and other reasons (tumour, osteoarthritis etc.) developments in prosthesis design and application have been reported to have resulted in significant reductions in loss of labour force and mortality [1-3]. The shoulder joint is one of the most mobile joints in the body and one of the joints most exposed to trauma. Industries established for the manufacture of prostheses have been primarily in economically developed countries such as the USA, Japan and the UK and with modern prosthesis production conforming to the latest developments, the products are marketed in many countries. The countries with a prosthesis industry design and manufacture prostheses primarily according to the morphometric data of the population of their own country.
However, these prostheses are used in populations of different ethnic and morphological structure and there is generally an incompatibility between the features of the prosthesis and the morphometric data of the population where they are used. As a result of this incompatibility and curettage of the bone structure, associated loss of tissue develops which has a negative effect on clinical progress and success [4,5]. These problems could be overcome if the countries with a prosthesis industry produced prostheses appropriate to the morphometric features of countries with different ethnic characteristics. High levels of patient satisfaction, excellent functional results, relief of pain and long survival have been reported in series of shoulder arthroplasty [6-8]. In parallel with these good results, an increasing number of shoulder arthroplasties are being applied in Turkey [9]. Loss of time, work force and costs are also reduced to a minimum. In this study of a Turkish population, a morphometric evaluation was made in a 2 dimensional environment of some parameters used in the design of proximal humerus prosthesis used in the shoulder region.
The aim of this study was to evaluate the effect on prognosis of morphometric features by measuring on Anteroposterior (AP) plain shoulder radiographs some parameters which are used in the design of proximal humerus prosthesis.
Materials and Methods
Study design
Approval for the study was granted by the Institutional Ethics Committee. In the period 2010-2015 anterior-posterior radiographs were taken because of shoulder pain in a total of 850 patients at Kirikkale University Medical Faculty Hospital, Turkey. In this retrospective clinical study, the plain shoulder radiographs were used of 195 (101 male (51.8%), 94 female (48.2%)) patients aged 18-65 years (mean age, 38.8 ± 11.5 years; males 35.4 ± 11.6 years, females 42.5 ± 10.2) with adhesive capsulitis, rotator cuff rupture and soft tissue trauma. Measurements were made on the radiograph of Head Height (HH), Frontal Base Diameter of the Head (FBD), 3 points at 3 cm intervals from proximal to distal of the medullar canal at the level of surgery Endosteal Diameter (ED1, ED2 and ED3 respectively), Neck-Shaft Angle (NSA) and Head-Neck Angle (HNA). In the radiographic measurements, the Radiant Viewer measurement program was used in a digital environment. The measurements were performed on radiographs obtained digitally using radiopacs media. The measurements were made by two authors (Both are radiologist). Intra and inter-observer error analysis was made. Standard error means are 0.754, 0.696 about HH, 0.629, 0.615 about FBD, 0.321, 0.308 about NSA, 0.284, 0.293 about HNA, 0.467, 0.433 about ED1, 0.397, 0.393 about ED2 and 0.388, 0,392 about ED3. Linear measurements were made with sensitivity to 1 mm and angular measurements were made with sensitivity to 0.1° using Radiant viewer own measurement program. Magnification range is 15% and correction factor is 1.09.
In the study, a total of 7 parameters were measured as 2 angular and 5 linear measurements. The definitions related to these parameters are given below.
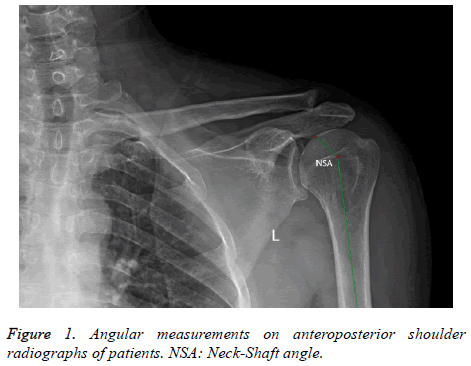
A) Angular measurements were stated in degrees (°): 1. NSA: Neck-shaft angle (Humeral inclination angle): Head inclination angle is defined as the inclination of the anatomic neck in the frontal plane. The angle was measured on the anteroposterior radiographic projection and was formed by the intersection of the axis of the proximal humerus and the line perpendicular to the neck axis (Figure 1).
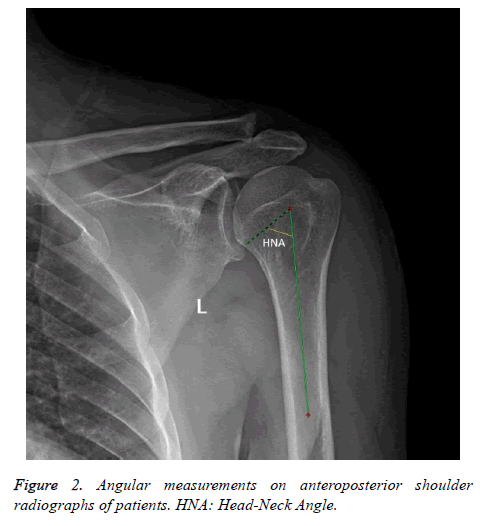
2. HNA: Head-neck angle: Head-Neck Angle was measured on the antero posterior radiographic projection and was formed by the intersection of the axis of the proximal humerus and the line perpendicular to the anatomic neck (Figure 2).
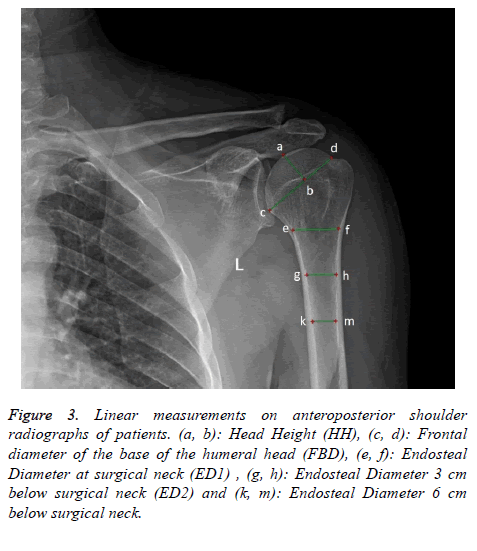
B) Linear parameters were stated in millimetres (mm): 1. HH: Head height: Head height determines the height or thickness of the humeral head and was measured in the anteroposterior radiographic projection (Figure 3).
Figure 3. Linear measurements on anteroposterior shoulder radiographs of patients. (a, b): Head Height (HH), (c, d): Frontal diameter of the base of the humeral head (FBD), (e, f): Endosteal Diameter at surgical neck (ED1) , (g, h): Endosteal Diameter 3 cm below surgical neck (ED2) and (k, m): Endosteal Diameter 6 cm below surgical neck.
2. FBD (Frontal base diameter): Frontal diameter of the base of the head: Frontal diameter of the base of the head is the diameter of the head segment at the anatomic neck and was measured in the anteroposterior radiographic projection. (Figure 3).
3. ED1: Endosteal Diameter at surgical neck (diameter of the medullar canal at the level of surgery in the neck) (Figure 3).
4. ED2: Endosteal Diameter 3 cm below surgical neck (diameter of the medullar canal 3cm below the level of surgery in the neck) (Figure 3).
5. ED3: Endosteal Diameter 6 cm below surgical neck (diameter of the medullar canal 6cm below the level of surgery in the neck) (Figure 3).
Statistical analysis
In the statistical analyses of the study, SPSS (Statistical Package for Social Sciences) for Windows 15.0 program was used. In the comparison of paired groups, Student’s t-test was used for parameters showing normal distribution. A value of p<0.05 was accepted as statistically significant. The cases were separated into 4 different age groups as males and females. A statistical comparison was made of the mean morphometric measurement values of same gender cases in different age groups. The groups were Group 1: 61 males aged 18-39 years, Group II: 30 female aged 18-39 years, Group III: 40 males aged ≥ 40 years and Group IV: 64 females aged ≥ 40 years. The mean and standard deviations were calculated for each parameter separately for males and females and for all cases. The mean measurement values were statistically compared between the genders regardless of age using the t-test. Parameters measured in other populations were statistically compared with the values obtained from the current study population. The results obtained were presented in table format.
Results
The data related to the results of the parameters measured in the study are presented in Table 1. The results of the measurements made for specific age groups are shown in Table 2. The results of the statistical test applied with the t-test to the parameter values of different age groups of the same gender are shown in Tables 3 and 4. In the comparison of Groups I and III, , the mean values of HH were 23.9 ± 2.61 in Group I and 22.7 ± 2.61 in Group III and the mean values of ED1 were measured as 22.1 ± 3.12 in Group I and 20.6 ± 3.01 in Group III and in other parameters, no statistically significant difference was determined. In the comparison of Groups II and IV, the mean values of FBD were 29.1 ± 3.72 in Group II and 30.5 ± 2.95 in Group IV and the mean values of ED1 were measured as 18.5 ± 2.59 in Group II and 13.7 ± 1.9 in Group IV and in other parameters, no statistically significant difference was determined. The results of the current study and those of studies of other populations based on the parameters measured in the current study are shown in Table 5.
| Age (Mean ± SD) | HH (mm) (Mean ± SD) | FBD (mm) (Mean ± SD) | ED1 (mm) (Mean ± SD) | ED2 (mm) (Mean ± SD) | ED3 (mm) (Mean ± SD) | NSA (degree) (Mean ± SD) | HNA (degree) (Mean ± SD) | |
|---|---|---|---|---|---|---|---|---|
| WOMEN (n=94) | 42.5 ± 10.2 | 20.5 ± 2.26 | 30.1 ± 3.27 | 19.2 ± 2.28 | 13.5 ± 2.06 | 11.3 ± 1.89 | 136.2 ± 3.53 | 43.7 ± 3.53 |
| MEN (n=101) | 35.4 ± 11.6 | 23.4 ± 2.67 | 32.5 ± 4.96 | 21.5 ± 3.16 | 15.4 ± 2.72 | 12.8 ± 2.39 | 136.5 ± 3.5 | 43.4 ± 3.5 |
| TOTAL (n=195) | 38.8 ± 11.5 | 22 ± 2.88 | 31.3 ± 4.39 | 20.4 ± 2.98 | 14.5 ± 2.6 | 12.1 ± 2.29 | 136.4 ± 3.5 | 43.5 ± 3.5 |
| HH: Head Height; FBD: Frontal Base Head; ED1: Endosteal Diameter at level surgical neck of humerus; ED2: Endosteal Diameter 3 cm below surgical neck; ED3: Endosteal Diameter 6 cm below surgical neck; NSA: Neck-Shaft Angle; HNA: Head-Neck Angle. | ||||||||
Table 1. General statistical results of measurements.
| Group I (n=61) (18-39 age men) | Group II (n=30) (18-39 age women) | Group III (n=40) (40 age and upper men) | Group IV (n=64) (40 age and upper women) | |
|---|---|---|---|---|
| MEAN ± SD | MEAN ± SD | MEAN ± SD | MEAN ± SD | |
| HH (mm) | 23.9 ± 2.61 | 20.3 ± 1.98 | 22.7 ± 2.61 | 20.5 ± 2.39 |
| FBD (mm) | 33.2 ± 4.06 | 29.1 ± 3.72 | 32.2 ± 3.18 | 30.5 ± 2.95 |
| ED1 (mm) | 22.1 ± 3.12 | 18.5 ± 2.59 | 20.6 ± 3.01 | 19.5 ± 2.05 |
| ED2 (mm) | 15.7 ± 2.62 | 12.9 ± 2.32 | 14.9 ± 2.83 | 13.7 ± 1.9 |
| ED3 (mm) | 13.2 ± 2.24 | 10.9 ± 2.04 | 12.4 ± 2.55 | 11.5 ± 1.79 |
| NSA (degree) | 136.3 ± 2.24 | 135.6 ± 4.21 | 136.8 ± 3.66 | 136.6 ± 4.01 |
| HNA (degree) | 43.6 ± 3.73 | 44.3 ± 4.21 | 43.1 ± 3.66 | 44.8 ±1 2.60 |
| HH: Head Height; FBD: Frontal Base Head; ED1: Endosteal Diameter at level surgical neck of humerus; ED2: Endosteal Diameter 3 cm below surgical neck; ED3: Endosteal Diameter 6 cm below surgical neck; NSA: Neck-Shaft Angle; HNA: Head-Neck Angle. | ||||
Table 2. General statistical results of measurements in different age and gender groups.
| Parameters | Group I (n=61) (18-39 age men) | Group III (n=40) (40 age and upper men) | P-value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| HH (mm) | 23.9 ± 2.61 | 22.7 ± 2.61 | 0.01 |
| FBD (mm) | 33.2 ± 4.06 | 32.2 ± 3.18 | 0.2 |
| ED1 (mm) | 22.1 ± 3.12 | 20.6 ± 3.01 | 0.01 |
| ED2 (mm) | 15.7 ± 2.62 | 14.9 ± 2.83 | 0.18 |
| ED3 (mm) | 13.2 ± 2.24 | 12.4 ± 2.55 | 0.11 |
| NSA (degree) | 136.3 ± 2.24 | 136.8 ± 3.66 | 0.51 |
| HNA(degree) | 43.6 ± 3.73 | 43.1 ± 3.66 | 0.52 |
| HH: Head Height; FBD: Frontal Base Head; ED1: Endosteal Diameter at level surgical neck of humerus; ED2: Endosteal Diameter 3 cm below surgical neck; ED3: Endosteal Diameter 6 cm below surgical neck; NSA: Neck-Shaft Angle; HNA: Head-Neck Angle. | |||
Table 3. Statistical analysis results between group I and group III.
| Parameters | Group II (n=30) (18-39 age women) | Group IV (n=64) (40 age and upper women) | P-value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| HH (mm) | 20.3 ± 1.98 | 20.5 ± 2.39 | 0.12 |
| FBD (mm) | 29.1 ± 3.72 | 30.5 ± 2.95 | 0.01 |
| ED1 (mm) | 18.5 ± 2.59 | 19.5 ± 2.05 | 0.01 |
| ED2 (mm) | 12.9 ± 2.32 | 13.7 ± 1.9 | 0.22 |
| ED3 (mm) | 10.9 ± 2.04 | 11.5 ± 1.79 | 0.13 |
| NSA (degree) | 135.6 ± 4.21 | 136.6 ± 4.01 | 0.51 |
| HNA (degree) | 44.3 ± 4.21 | 44.8 ±1 2.60 | 0.53 |
| HH: Head Height; FBD: Frontal Base Head; ED1: Endosteal Diameter at level surgical neck of humerus; ED2: Endosteal Diameter 3 cm below surgical neck; ED3: Endosteal Diameter 6 cm below surgical neck; NSA: Neck-Shaft Angle; HNA: Head-Neck Angle. | |||
Table 4. Statistical analysis results between group II and group IV.
| Authors/Country | McPherson et al./USA | Michael et al./U.S.A | Jennifer et al./USA and UK | Ralph et al./Switzerland | Bakir et al./Sweden | Fraser et al./Scotland | Zhang et al./China | Katsumi et al./Japan | İyem et al./Turkey (Current study) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Method | On AP X-ray | On AP X-ray | An electromagnetic tracking system | Directly onspecimens | On AP X-ray | Directly on specimens | on 3D CT | On AP X-ray | On AP X-ray | |||
| Number of cases | 93 | 21 | 28 | 200 | 70 | 24 | 180 | 471 | 195 | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||||
| Parameters | HH (mm) | 47.6 ± 4.8 | 18.5 ± 2 | Left | 15.4 ± 1 | 17 ± 1.7 | 20 ± 3 | 16.9 ± 1.5 | 16.7 ± 1.9 | 22 ± 2.88 | ||
| Right | 14.5 ± 0.9 | |||||||||||
| FBD (mm) | 48.8 ± 3.2 | 54.3 ± 5.4 | 31.3 ± 4.39 | |||||||||
| ED1 (mm) | 42.7 ± 7.9 (Neck) | Mean of all sides engaged (12.7 ± 1.7) | Best-fitting cylinder (11.5 ± 2.09) | 20.4 ± 2.98 | ||||||||
| ED2 (mm) | 16 ± 3.7 ( Below 5 cm) | 14.5 ± 2.6 | ||||||||||
| ED3 (mm) | 15.3 ± 2.6 (Below 10 cm) | 12.1 ± 2.29 | ||||||||||
| NSA (degree) | 141° ± 8.6 | Left | 132.9° ± 2.9 | 137° ± 3.62 | 133° ± 6 | 135.0° ± 4.4 | 132.4° ± 4.7 | 140.4° ± 4.1 | 136.4° ± 3.5 | |||
| Right | 132.8° ± 4.4 | |||||||||||
| HNA (degree) | 40.7° ± 4.7 | 43.5° ± 3.5 | ||||||||||
| HH: Head Height; FBD: Frontal Base Head; ED1: Endosteal Diameter at level surgical neck of humerus; ED2: Endosteal Diameter 3 cm below surgical neck; ED3: Endosteal Diameter 6 cm below surgical neck; NSA: Neck-Shaft Angle; HNA: Head-Neck Angle. | ||||||||||||
Table 5. Data of the articles related with parameters.
Discussion
The application of shoulder prosthesis started in 1973 with the Monoblock prosthesis (3M, Paul, MN, USA) [7,8]. There was limited information at that time about significant changes in the normal humerus anatomy. Since then, many studies have described the size of the humerus head in normal individuals, the neck-shaft angle, the presence of retroversion variations and that there could be pathological offset [6,10-12]. Modular designs (2nd and 3rd generation) have been developed to increase as much as possible the compatibility with the normal biological mechanics of the shoulder and these variations [13]. In several biomechanical studies, it has been shown that better restoration of the normal anatomy and better clinical results could be obtained with the use of a modular prosthesis design [14-16].
Morphological differences between populations demand changes in prosthesis design. Therefore, the manufacture of prosthesis compatible with the morphological structure of every population would be a factor increasing the functionality of the prosthesis. Clear information related to the anatomic connections and bone anatomy of the normal proximal humerus and glenoid region is important for prosthesis design [17]. Data of the dimensions of the proximal humerus are important for the appropriate design of a prosthetic humeral component [10]. When using a prosthetic implant with a varying incline, the surgeon has a limited number of head dimension alternatives. If there is any incompatibility between the measurements and local head dimensions in prostheses which can be used, there will be restricted anatomic matching. In addition, any prosthesis system outside the range of anatomic prosthesis options, will not allow an infinite number of special positions [18].
This study is of value in that compatibility to normal anatomic structure and the selected and measured parameters are taken into consideration in the design of shoulder prosthesis. The indicator for the choice of these parameters was their importance in clinical use. In the application of shoulder prosthesis, Head Height is important in providing compatibility of the humeral component with the glenoid component in all 3 axes (vertical, transverse and sagittal). An inappropriate size prosthesis may cause restriction of head height shoulder movements and subluxation [10,17-20]. In the application of shoulder arthroplasty, head base frontal diameter affects humeral head resection and the movements in the transverse axis of the prosthesis head [10]. In studies conducted on other populations, with the exception of a study of 93 cases by McPherson (HH: 47.6 ± 4.8 mm), the other HH measurement values were below the mean value of 22 ± 2.88 mm measured in the current study (Table 5) [17].
The endosteal diameter is an important parameter used in the determination of the dimensions within the intra-medullar canal of the humeral stem. A suitably prepared humeral stem of sufficient thickness and length is extremely important in the provision of postoperative prosthesis stabilisation. Errors in measurement in this section may cause humeral shaft fractures and prosthesis loosening. Humeral stem diameters have been classified by international prosthesis manufacturers. According to Zimmer, humeral stem diameters are classified as 6-8 mm small, 9-11 mm medium, 12-14 large and>15 mm extra-large.
According to this, humeral stem lengths vary between 130 mm-170 mm. The reason for the selection of endosteal diameters at 3 and 6 cm from the surgical neck level used in this study was related to the use of 9-12 cm length generally from the resection section for the prosthesis head of the humeral stems [17-20]. In the data shown in Table 5 of the data of research conducted on other populations, in a study of 93 cases by McPherson et al. the endosteal diameter of the most distal section (ED3) was measured as mean 15.3 ± 2.6 mm, in a study of 21 cases by Michael as 12.7 ± 1.7 mm, and in a study of 200 cases by Ralph et al. as 11.5 ± 2.09 mm. When the values obtained in the current study were examined, the most distal Endosteal Diameter (ED3) was determined as mean 12.8 ± 2.39 mm in males and 11.3 ± 1.89 mm in females.
In shoulder arthroplasty applications, NSA is a very important parameter in determining the valgus and varus angle of the prosthesis and providing the extent of the angular movement in the shoulder joint. However, attention must be paid to provide compatibility between the humeral head and the glenoid cavity [10,13,17-20]. In the data related to NSA shown in Table 5, the NSA was measured as between 132° and 141° in studies conducted on other populations and as mean 136.4° ± 3.5° in the current study.
A decrease in HNA in shoulder prosthesis application causes pain and limitation of joint movement by creating pressure on the lateral angular section of the scapula when the humerus calcar section of the shoulder joint is in adduction. In this respect, the use of this parameter in surgery is important [13,21,22]. In the data related to HNA shown in Table 5, the HNA was measured in only one study and was mean 40.7° and 4.7° and was measured as mean 43.5° ± 3.5° in the current study.
The failure of many existing shoulder replacement systems to develop the proximal humeral geometry is responsible for some complications related to shoulder arthroplasty [19]. Using different stem fixation techniques, the possibility of choice of size of humeral head components and non-anatomic stem design prostheses for the removal of different symptoms offers the surgeon the use of a wide range of partial shoulder prosthesis options [23]. To ensure a regular head size and avoid varus or valgus humeral head inclination, defining the straight cut bone level is a critical step [24].
A previous study reported that the dimensions of an osteotomised humeral head would be useful in correcting errors for an ideal implant design [25]. In a study conducted in China, the results of 3 dimensional measurements were reported to be helpful in preventing large bone losses in surgical applications [26]. A Japanese study stated that it was necessary to pay attention to tissue impingement developing associated with a reduced angle of humeral inclination and weakening abductor muscle [27].
The aim of this study was not to recommend any new method or application technique for shoulder prosthesis applications. The aim was to identify that there are differences in the morphometric data of each population and that taking these differences into consideration in prosthesis applications will contribute to the success of the prosthesis. In Table 5, the results of the current study are compared with the results of studies conducted on populations with ethnic differences such as England, the USA, some African countries, China and Japan. The HH measurement of the current study sample was higher, whereas the NSA value was similar to that of some European countries but differences were seen compared to the other populations. These results showed that each population has differences in the morphometric data of the proximal humerus. For postoperative success, prosthesis design must take these differences into consideration.
In the comparison of the measured parameters of the current study of the male cases in different age groups, it was observed that in those aged 40 years and over, there was a decrease in humeral head height and endosteal diameter at surgical neck level. In contrast, in the comparison of the different age groups of the female cases, an increase was seen in humeral head height and endosteal diameter at surgical neck level in those aged 40 years and over. These differences were not statistically significant in either gender. It is thought that these results could have originated from differences in height weight and body mass index.
Limitations of this study can be said to be that the number of cases in the sample examined was low and there was no facility for the evaluation of 3 dimensional imaging.
In conclusion, the differences between populations in the parameters defined in this study, which are used for the design of shoulder prosthesis humeral component, could form a database for prosthesis manufacture. In addition, when the results of the study are examined in detail in respect of complications on the basis of these parameters, the head-neck ratio must be greater than 1/3 and the HH must be compatible with the glenoid cavity surface. In respect of the angles, care must take that the NSA and HNA values are calculated correctly as an excessive varus angle could lead to the development of impingement in adduction and an excessive valgus angle, to subluxation. Compatibility of the endosteal diameter and humeral stem is important for the prevention of prosthesis loosening and humeral shaft fractures which may develop intra-operatively or postoperatively.
References
- Boileau P, Sinnerton RJ, Chuinard C, Walch G. Arthroplasty of the shoulder. J Bone Joint Surg Br 2006; 88: 562-575.
- Milner GR, Boldsen JL. Humeral and femoral head diameters in recent white American skeletons. J Forensic Sci 2012; 57: 35-40.
- Somesh MS, Prabhu LV, Shilpa K, Pai MM, Krishnamurthy A, Murlimanju BV. Morphometric study of the humerus segments in Indian population. Intern J Morphol 2011; 29: 1174-1180.
- Cay N, Tosun A, Doayan M, Karaoaylanoaylu M, Bozkurt M. The effect of morphometric relationship between the glenoid fossa and the humeral head on rotator cuff pathology. Acta Orthop Traumatol Turc 2012; 46: 325-331.
- Kilic M, Berth A, Blatter G, Fuhrmann U, Gebhardt K, Rott O. Anatomic and reverse shoulder prostheses in fracture sequelae of the humeral head. Acta Orthop Traumatol Turc 2010; 44: 417-425.
- DeLude JA, Bicknell RT, MacKenzie GA, Ferreira LM, Dunning CE. An anthropometric study of the bilateral anatomy of the humerus. J Shoulder Elbow Surg 2007; 16: 477-483.
- Neer CS 2nd. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am 1974; 56: 1-13.
- Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am 1982; 64: 319-337.
- Godeneche A, Boileau P, Favard L, Le Huec JC, Levigne C. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: early results of 268 cases. J Shoulder Elbow Surg 2002; 11: 11-18.
- Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elbow Surg 2002; 11: 331-338.
- Iannotti JP, Gabriel JP, Schneck SL, Evans BG, Misra S. The normal glenohumeral relationships. An anatomical study of one hundred and forty shoulders. J Bone Joint Surg Am 1992; 74: 491-500.
- Roche C, Angibaud L, Flurin PH, Wright T, Fulkerson E. Anatomic validation of an anatomic shoulder system. Bull Hosp Jt Dis 2006; 63: 93-97.
- Pearl ML. Proximal humeral anatomy in shoulder arthroplasty: Implications for prosthetic design and surgical technique. J Shoulder Elbow Surg 2005; 14: 99-104.
- Harryman DT, Sidles JA, Harris SL, Lippitt SB, Matsen F. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. A study in cadavera. J Bone Joint Surg 1995; 77: 555-563.
- Nyffeler RW, Sheikh R, Jacob HA, Gerber C. Influence of humeral prosthesis height on biomechanics of glenohumeral abduction. An in vitro study. J Bone Joint Surg Am 2004; 86-86A: 575-580.
- Williams GR, Wong KL, Pepe MD, Tan V, Silverberg D, Ramsey ML. The effect of articular malposition after total shoulder arthroplasty on glenohumeral translations, range of motion, and subacromial impingement. J Shoulder Elbow Surg 2001; 10: 399-409.
- McPherson EJ, Friedman RJ, An YH, Chokesi R, Dooley RL. Anthropometric study of normal glenohumeral relationships. J Shoulder Elbow Surg 1997; 6: 105-12.
- Pearl ML, Kurutz S, Postachini R. Geometric variables in anatomic replacement of the proximal humerus: how much prosthetic geometry is necessary? J Shoulder Elbow Surg 2009; 18: 366-370.
- Wirth MA, Ondrla J, Southworth C, Kaar K, Anderson BC, Rockwood CA. Replicating proximal humeral articular geometry with a third-generation implant: a radiographic study in cadaveric shoulders. J Shoulder Elbow Surg2007; 16: 111-116.
- Jeong J, Jung HW. Optimizing intramedullary entry location on the proximal humerus based on variations of neck-shaft angle. J Shoulder Elbow Surg 2015; 24: 1386-1390.
- Sano H, Kamimura M, Oizumi A, Isefuku S. Secondary subacromial impingement after valgus closing-wedge osteotomy for proximal humerus varus. Case Rep Orthop 2015; 2015: 652096.
- Wu CH, Ma CH, Yeh JJH, Yen CY, Yu SW, Tu YK. Locked plating for proximal humeral fractures: differences between the deltopectoral and deltoid-splitting approaches. J Traum Acut Care Surg 2011; 71: 1364-1370.
- Foruria A, Antuña S, Rodríguez-Merchan E. Shoulder hemiarthroplasty: review of basic concepts. Revista espanola de cirugia ortopedicay traumatologia (English edn.) 2008; 52: 392-402.
- Kadum B, Hassany H, Wadsten M, Sayed-Noor A, Sjoden G. Geometrical analysis of stemless shoulder arthroplasty: a radiological study of seventy TESS total shoulder prostheses. Int Orthop 2015; 1-8.
- Harrold F, Wigderowitz C. Humeral head arthroplasty and its ability to restore original humeral head geometry. J Shoulder Elbow Surg 2013; 22: 115-121.
- Zhang L, Yuan B, Wang C, Liu Z. Comparison of anatomical shoulder prostheses and the proximal humeri of Chinese people. J Eng Med 2007; 221: 921-927.
- Takase K, Yamamoto K, Imakiire A, Burkhead WZ Jr. The radiographic study in the relationship of the glenohumeral joint. J Orthop Res 2004; 22: 298-305.