Case Report - Ophthalmology Case Reports (2023) Volume 7, Issue 4
A case of Bilateral Third Cranial Nerve Palsy due to Bilateral Thalamic Infarcts
Haritha Vasudevan*, Virna M. Shah, Jassim Koya
Department of Ophthalmology, Aravind Eye hospital, Coimbatore, India
- *Corresponding Author:
- Haritha Vasudevan
Department of Ophthalmology
Aravind Eye hospital, Coimbatore, India
E-mail: harithavasudev29@gmail.com
Received: 24-May-2023, Manuscript No. OER-23-109431; Editor assigned: 26-May-2023, Pre QC No. OER-23-109431 (PQ); Reviewed: 05-Jun-2023, QC No. OER-23-109431; Revised: 27-Jul-2023, Manuscript No. OER-23-109431 (R); Published: 03-Aug-2023, DOI: 10.35841/oer-7.4.164
Citation: Vasudevan H, Shah VM, Koya J. A case of bilateral third cranial nerve palsy due to bilateral thalamic infarcts. Ophthalmol Case Rep. 2023; 7(4):164.
Abstract
Purpose: To report a case of bilateral third cranial nerve palsy which is not a common presentation in the standard neuro-ophthalmology clinic, a subset of its various etiologies is immediately life-threatening to the patient and requires through evaluation. A rare case of bilateral complete third nerve palsy with pupillary involvement due to an Artery of Percheron (AOP) infarct in a 70-year-old male patient presenting to a neuro-ophthalmology clinic is reported here. Methods: The patient presented to the ophthalmology clinic and reported a 3-day history of bilateral progressive drooping of upper eyelids, associated with a history of altered level of consciousness from a transient ischemic attack occurring at the time of onset of the primary complaints. Severe ptosis was seen in both eyes with negative fatigability. Both pupils were mid-dilated and fixed. Eye movement examination revealed bilateral restricted elevation and extorsion with mild restriction of adduction and intorsion suggestive of third cranial nerve palsy of both eyes. He was diagnosed to have bilateral oculomotor palsy with pupil involvement, and urgent neuroimaging was done. His MRI brain with cervical and cerebral MRA revealed acute infarcts in both thalami (right >left side) due to infarction of the AOP. Results: Patient was immediately transferred to the emergency room for management by the neurology department. The AOP infarct was thrombolyzed, and patient was further managed with anticoagulants, lipid lowering agents. Conclusion: Pupil-involving third-nerve palsy warrants thorough investigation to investigate a vascular or compressive root cause. The significance of this case is to acknowledge the rarity of this commonly overlooked infarction; to differentiate an AOP infarction from a basilar artery infarction and the rare neuro-ophthalmic presentation of this patient to increase awareness amongst physicians.
Keywords
Bilateral oculomotor nerve palsy, Bilateral thalamic infarct, Artery of percheron.
Introduction
Bilateral thalamic infarcts are relatively uncommon and occur in 20 to 25% of all thalamic strokes, and in about 0.6% of all acute ischemic strokes, which results in a vast range of neurologic and neuropsychologic manifestations [1-3]. Thalamic infarctions are of great concern to not only neurologists but also to ophthalmologists due to its many debilitating neuro-ophthalmologic deficits including visual, pupillary, oculomotor and eyelid abnormalities, which greatly affect patients’ daily living [3,4].
While bilateral third cranial nerve palsy is not such a common presentation in the standard neuro-ophthalmology clinic, a subset of its various etiologies is immediately life-threatening to the patient and requires through evaluation [5]. We report a rare case of bilateral complete third nerve palsy with pupillary involvement due to an Artery of Percheron (AOP) infarct in a 70-year-old male patient presenting to a neuro-ophthalmology clinic.
Case description
The consent form has been taken from the patient and there is no need to attach the image.
A 70-year-old male presented to the ophthalmology clinic and reported a 3-day history of bilateral progressive drooping of upper eyelids, associated with a history of altered level of consciousness from a transient ischemic attack occurring at the time of onset of the primary complaints. The patient denied complaints of headache, vomiting, slurring of speech, facial asymmetry, limb weakness, fever or history of trauma. The past medical history was remarkable for systemic hypertension on treatment for 10 years. His social history included tobacco smoking and chronic alcohol consumption for more than 40 years. The review of systems was unremarkable.
The Best Corrected Visual Acuity (BCVA) was 6/6 in the right eye and 6/9 in the left eye. Severe ptosis was seen in both eyes with negative fatigability. Both pupils were mid-dilated and fixed. Eye movement examination revealed bilateral restricted elevation and extorsion with mild restriction of adduction and intorsion suggestive of third cranial nerve palsy of both eyes. The slit-lamp and fundus examination were otherwise normal in both eyes. The other cranial nerve examination was normal in addition to the higher function tests, motor and sensory system, and cerebellar function tests.
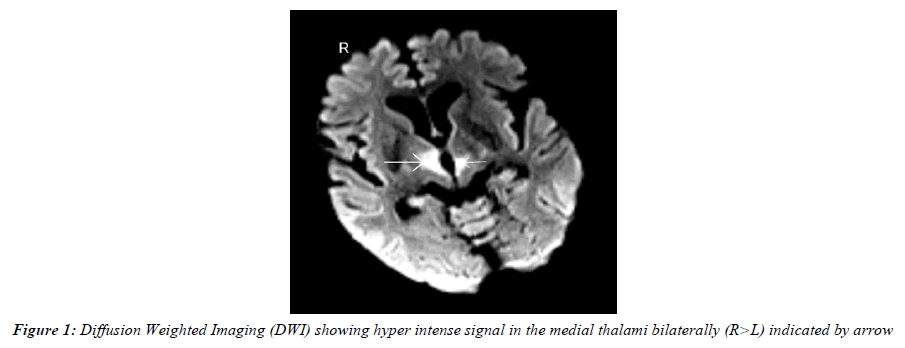
The patient’s blood sugar, coagulation profile, complete blood count, ESR and serum electrolytes were within normal limits. His lipid profile suggested a case of dyslipidemia. He was diagnosed to have bilateral oculomotor palsy with pupil involvement, and urgent neuroimaging was done. His MRI brain with cervical and cerebral MRA revealed acute infarcts in both thalami (right >left side) due to infarction of the Artery of Percheron (Figure 1). Basilar artery occlusion was excluded based on patency of basilar and posterior cerebral arteries on patient MRA. Patient was immediately transferred to the emergency room for management by the neurology department. The AOP infarct was thrombolyzed, and patient was further managed with anticoagulants, lipid lowering agents. On cardiac evaluation, he was found to have paroxysmal atrial fibrillation and was started on calcium channel blockers. At the 2-week follow-up, residual bilateral complete third nerve palsy was noted. He was advised to complete extraocular movement physiotherapy, continue medications as per the neurologist’s advice, and be on regular follow-up with us at the neuro-ophthalmology clinic.
Discussion
Isolated cranial nerve palsy is a significant neurological entity as microvascular ischemia is the presumed cause in patients with atherosclerotic and cardio embolic risk factors. Among all cases of ocular misalignment from cranial nerve palsies, third nerve palsies are critical because a subset of these is caused by life-threatening aneurysms and infarctions [5]. Oculomotor nerve palsy is a common symptom of midbrain infarctions, but studies have reported cases of paramedian thalamic infarction inducing third-nerve palsy without a definite lesion of the brainstem [3].
Thalamus infarction typically presents with a triad of oculomotor abnormalities, cognitive abnormalities, and alterations in consciousness [1]. Our patient reported alteration of consciousness at the onset of symptoms, which is classic for thalamic infarcts.
An occlusion in artery of Percheron, which is a rare anatomical variant arising from proximal posterior cerebral artery, between basilar artery and posterior communicating artery can affect various thalamic nuclei and also rostral midbrain; can result in various clinical manifestations [2].
Our patient’s neuroimaging showed occlusion of AOP likely from cardio embolism, which gives rise to the characteristic pattern of bilateral paramedian thalamic infarcts, with or without rostral midbrain infarction. Some of the risk factors of stroke causing thromboembolism include atherosclerosis, atrial fibrillation (probable in this case), ventricular wall aneurysms, right-to-left shunts as well as hypercoagulable states, severely reduced left ventricular function, and vasoconstriction [1].
Conclusion
To our knowledge, this is the first case of a rare bilateral thalamic infarct of the rarer Artery of Percheron manifesting as bilateral, complete third nerve palsy with pupillary involvement. While we found some of the classical clinical characteristics mentioned previously in literature, this patient presented with pupil-involving oculomotor nerve palsy due to bilateral thalamic infarcts, caused due to AOP infarction and was found to have paroxysmal atrial fibrillation.
The significance of this case is to acknowledge the rarity of this commonly overlooked infarction; to differentiate an AOP infarction from a basilar artery infarction and the rare neuro- ophthalmic presentation of this patient to increase awareness amongst physicians.
References
- Kumral E, Evyapan D, Balk?r K, et al. Bilateral thalamic infarction: clinical, etiological and MRI correlates. Acta Neurol Scand. 2001;103(1):35-42.
- Cassourret G, Prunet B, Sbardella F, et al. Ischemic stroke of the artery of Percheron with normal initial MRI: a case report. Case reports in medicine. 2010;2010.
- Moon Y, Eah KS, Lee EJ, et al. Neuro-ophthalmologic features and outcomes of thalamic infarction: a single-institutional 10-year experience. J Neuroophthalmol. 2021;41(1):29-36.
- Adamec I, Barun B, Mahovi? Lakuši? D, et al. Neuro-ophthalmologic manifestations of thalamic stroke. Neuro-Ophthalmol. 2011;35(3):121-4.
- Lazaridis C, Torabi A, Cannon S. Bilateral third nerve palsy and temporal arteritis. Arch Neurol. 2005;62(11):1766-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref