Research Article - Ophthalmology Case Reports (2017) Volume 1, Issue 2
A case of bilateral pigment epithelial detachments with different treatment approaches with a Vegf inhibitor and Intraocular Dexamethasone
Hudson de Carvalho Nakamura*
Department of Ophthalmology, university of Eye Bank Foundation Goias, Brazil
- *Corresponding Author:
- Hudson de Carvalho Nakamura
Department of Ophthalmology, University of Eye Bank Foundation Goias, Brazil
Tel: +556283427777
E-mail: hudson.nakamura@alumni.utoronto.ca
Accepted date: January 16, 2018
DOI: 10.35841/ophthalmology.1.2.32-37
Visit for more related articles at Ophthalmology Case ReportsAbstract
we show a case of age related macular degeneration treated with Lucentis in the left eye for sixtimes, that failed and worsened after all sessions, and developed a recurrent occult neovascular membrane, a case that came from another eye center service, where they failed to switch to a different drug in an appropriate time, worsening the outcome to that one eye (left). The patient came to us in our service and the symptoms started in the better visual acuity eye (right) recently,and we promptly started the treatment, with Intraocular Dexamethasone Implant. We did not let the other eye without attention, despite the worse visual and anatomic outcome, also treated with a switch from Lucentis to Aflibercept. Both eyes had excellent results, even though the right eye recurred after a while and we used the same treatment due to good results at first (the membrane reactivated), and was treated again with the same medication (dexamethasone implant) and the chronic eye (left) was treated again, as well with Aflibercept, not because of recurrence, but because that one eye had an excellent anatomic resolution of the pigment epithelial detachment. After the second treatment, the left eye got better and did not worsen.
Keywords
Age related macular degeneration, choroidal neovascularization, vascular endothelial growth factor, intraocular injections.
Abbreviations
OCT: Optical Coherence Tomography, FA: Fluorescein Angiography, AMD: Age Related Macular Degeneration, CNV: Choroidal Neovascularization, VEGF: Vascular Endothelial Growth Factor, PDT: Photodynamic Therapy, PEDF: Pigment Epithelium Derived Factor, RPE: Retinal Pigment Epithelium, FDA: Food and Drug Administration, OCT: Ocular Computerized Tomography, FA: Fluorescein Angiography, OCTA: Oct Angiography, PDGFR: Protein Derived Growth Factor Receptors, PDGF: Protein Decided Growth Factor, PV: Polyploidy Vasculopathy.
Introduction
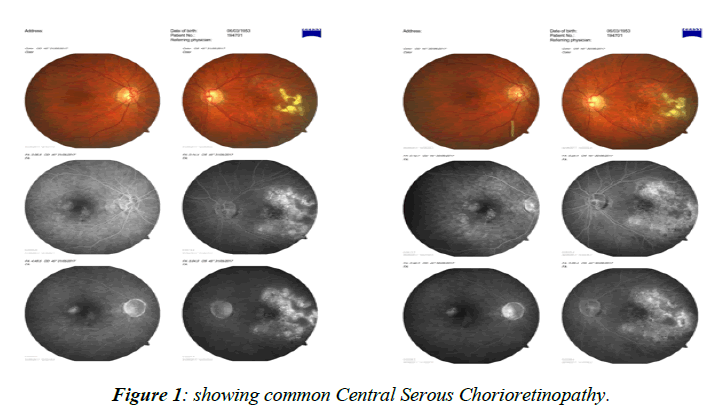
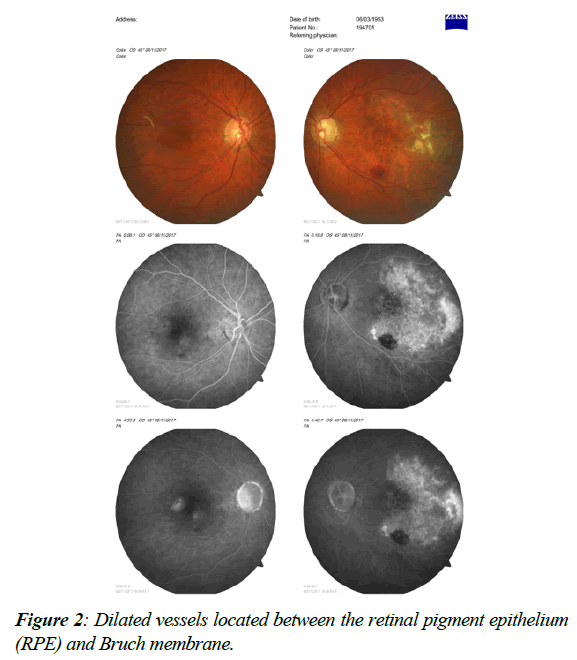
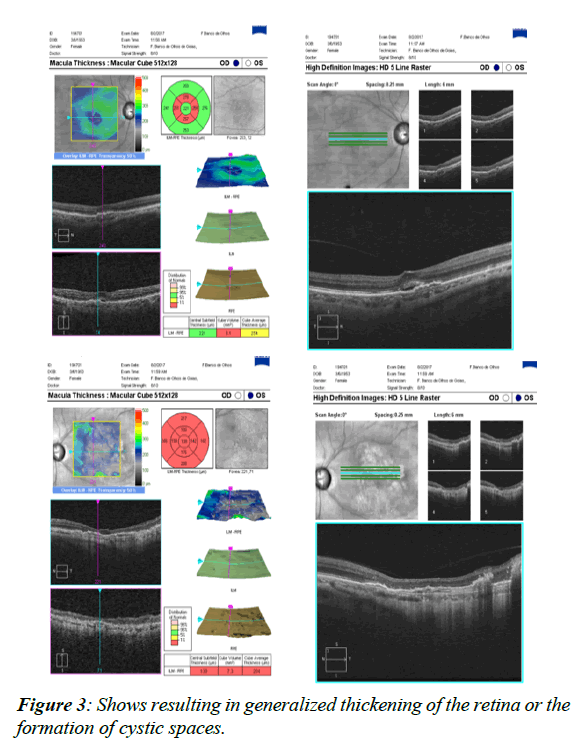
The treatment modalities came such as Photo Dynamic Therapy (PDT) with verteporfin and Transpupillary Thermo Therapy (TTT) [1] more recently intraocular injections for Vascular Endothelial Growth Factor (VEGF) inhibition and intraocular implant with dexamethasone, the latter far better than the corticoid used years ago solely for the treatment of some maculopathies such as cystoid macular edema and other diseases [2-4], such as uveitic macular edema So the development of pharmacological treatment for the membrane came to many evolving drugs used in ophthalmology today, starting with pegaptanib sodium (Macugen), this first one currently out of market, and other drugs under many current studies such as bevacizumab (Avastin). Ranibizumab (Lucentis) is also an option and Aflibercept (Eylia) was approved and being used in many clinical protocols [5]. The patient with PED (pigment epithelial detachment), which could be a signal of occult choroidal neovascular membrane [6-8] in the scope of age related macular degeneration also makes the treatment even more difficult and the differential diagnosis often times combines diseases such as Polypoid Vasculopathy and even the very common Central Serous Chorioretinopathy in Figure 1, many times thought as a diagnosis but, as we advanced with better diagnostic tools, to state OCT-A (Optical Coherence Tomography Angiography), it is shown that for many times could be actually be mistaken for a choroidal neovascular membrane. Still used today is indocyanine green angiographyAge-related macular degeneration (AMD) is a leading cause of visual impairment in the world. It’s worse complication, the choroidal neovascular membrane, especially in the sub macular form, usually affects life quality and functional development of one who does not seek for the appropriate treatment in due time. In the past, the membrane was treated with laser photocoagulation, backed up by the MPS (Macular Photocoagulation Study) [9], and many eyes had the membrane treated irrespective of the low visual acuity that could actually result, knowing that after some time the vision would get somehow better, as well as the contrast sensitivity, but this treatment today is considered out of date and it is no longer performed which discarded in our case polypoidal choroidal vasculopathy (PCV), one important differential to this case, which presents as a serosanguinous maculopathy, being a variant of neovascular age related macular degeneration. PCV was described as a type 1 choroidal neovascularization (CNV) [10-12] with or without a branching vascular network with polypoidal dilated vessels located between the retinal pigment epithelium (RPE) and Bruch membrane (Figure 2) [13]. Severe visual acuity loss may occur in patients secondary to repeated exudation episodes, scarring, hemorrhages, fibrosis, and others. The pathophysiology of AMD includes diffuse thickening of the inner aspect of Bruch's membrane associated with soft drusen and are often times accompanied by abnormalities of the Retinal Pigment Epithelium (RPE) with focal hyperpigmentation [14-16]. In exudative neovascular AMD, three patterns of Choroid Neovascularization (CNV) have been defined growth into the plane between the RPE and Bruch's membrane type 1 growth between the retina and RPE (type 2) [17] and retinal angiomatous proliferation within the retina type 3 Serum and blood leak from these fenestrated vessels and separate Bruch's membrane, the RPE and the retina from each other, leading to the accumulation of intraretinal fluid, resulting in generalized thickening of the retina or the formation of cystic spaces (Figure 3), causing the photoreceptors to become misaligned, and eventually degenerative changes occur with cell loss and eventual fibrosis [18-24].
Materials and Methods
Patient had two intraocular Aflibercept injections in the left eye and two Intravitreal Dexamethasone implant in the right eye; all procedures occurred with only topic anesthesia. On March 6, 2007 Patient had normal visual acuity, 20/20 OU. The intraocular pressures were 21 and 22, in OD and OS, respectively and the retinas were normal. On February 24, 2011 Patient already diagnosed as glaucoma, on treatment. Dec21 2012 Patient already diagnosed as glaucoma, on treatment. May, 2017 the Patient with 64 years old complained of metamorphosis in the right eye for four months. He came after a long time in another retinal service, where treatment for the left eye, to state six intraocular injections of Ranibizumab, with no good visual acuity [25]. The visual acuity at that time was 20/80 and counting fingers, respectively, with best correction. Intraocular pressures were normal, and the patient was being treated for glaucoma, with glaucoma drops. We promptly indicated for the patient Intravitreal Dexamethasone to the right eye, because we knew the past ocular history of anti-vega medication and bad result for the left eye (Ranibizumab), and also indicated Aflibercept for the left eye, which has a worse outcome and only counting fingers vision, as the “switch” medication for the pigment epithelial detachment [26]. Also we asked for OCT (Ocular Coherence Tomography), ICG (Indocyanin Green) and OCT-A (OCT-angiography) to discard Polypoid vasculopathy (PCV). On May 31, we had color and angiography images from the patient, showing a right pigment epithelial detachment with pooling hyper fluorescence and left multiple pigment epithelial detachments with diffuse leaks.
Evolution and Results
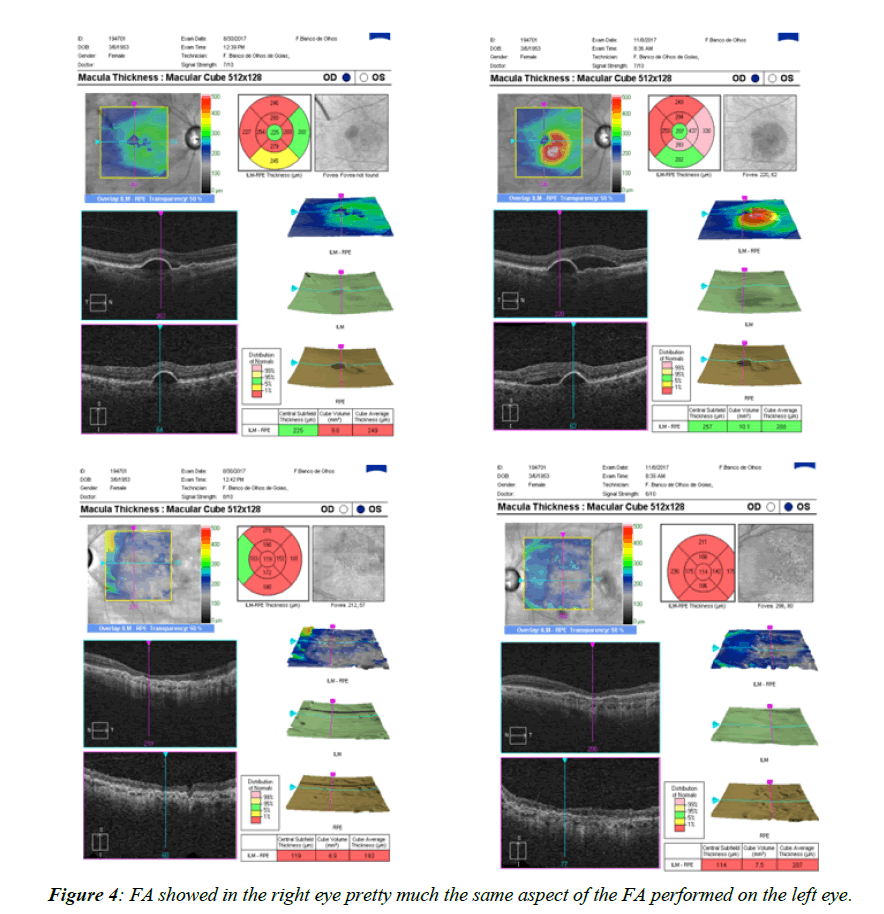
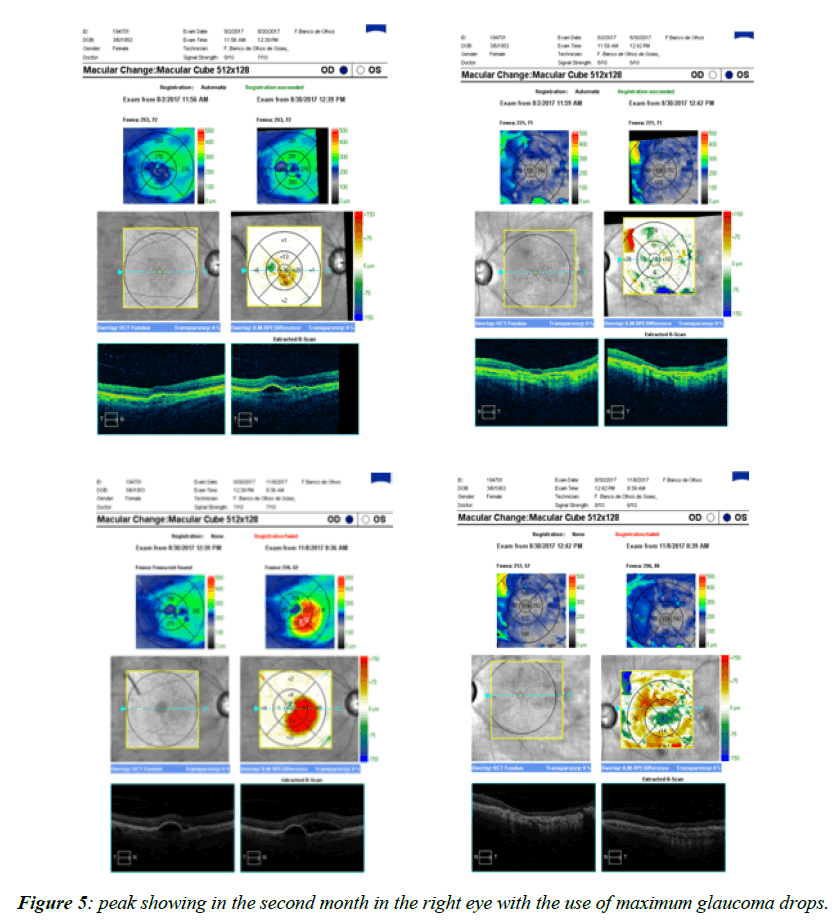
THE OCT showed On June7, 2017, the patient had intraocular Dexamethasone in the right eye, and had an excellent result. On June14 2017, flibercept was injected in the left eye; two months later, because the multiple PEDs reduced, we decided to inject again, on August 3, 2017. On August 30, 2017 [27-29], we compared both angiography and OCTs from August 2 and 30, 2017, and noticed that the left eye got stable, but the right eye had the membrane recurred, coming back to 20/80. We measured the best corrected visual acuity, and it was amazingly 20/30-3 in the right eye, on August 31, 2017 [30]. On July28 2017, the patient brought ICG, resulting in RPE rarefaction and resorbing sub-retinal hemorrhage. We actually doubted that diagnosis and relied only upon the images, because the exam was performed from another doctor in another service, so he did not see the patient, just reported the images from the ICG. On August 2, 2017, the Oct showed a complete resolution of the macular PED, but there was some concern about a possible vitreo-macular traction [31-33]. On August 3, 2017, the patient had intraocular Eylia Injection in the left eye. The right eye visual acuity was 20/50, and the left eye was counting fingers. On August 30, 2017, the OCT showed right eye recurrence and the left eye did not show any recurrence On August 30, 2017, the FA showed in the right eye pretty much the same aspect of the FA performed on May 31 (Figure 4), 2017 and the left eye did not show any recurrence. We could actually see the intraocular implant of dexamethasone floating in the inferior nasal part of the retina [34]. On August 31, 2017, the right visual acuity was 20/30. On September 6, 2017, the right best corrected visual acuity was 20/40-2. On November 8, 2017, in the right eye, we performed another OCT and found out pretty much the same shape, as compared to the exam from August 30, 2017, but since the visual acuity dropped to 20/80 in the right eye, we performed another Intravitreal Dexamethasone, the second implant, with visual acuity a lot better in the better eye (right), coming back to 20/50. On November 29, and another OCT exam was ordered but not yet performed. We decided not to perform another Elyria for the left eye, since it was stable. On December 20, the visual acuity got quite better, measured 20/50+2 [35-37]. The intraocular pressure in all visits varied from 18 to 25, with a peak showing in the second month in the right eye with the use of maximum glaucoma drops (Figure 5) (eye that had intravitreal dexamethasone implant), and was stable after that peak period, maintaining normal intraocular pressure even after the second dexamethasone implant to the right eye. The left eye did not have major concerns on the intraocular pressure all over the follow up period [38].
Conclusion
The main conclusion we arrived at from this study is that we need to analyze all treatment options available for pigment epithelial detachment, as well as compare earlier treatments, taking into consideration the patient history and response to other treatments We observed that the switch between drugs is an important issue to consider as we applied to this case the switching of ranibizumab (performed in another service) to aflibercept (performed by us), and the decision to start intravitreal dexamethasone to the right eye (not to repeat the use of anti-Vegf that gave a bad result to the patient in the past, when treated as explained above) both drugs performed their tasks the best, and we keep on with the same treatment knowing the switch was well performed, thus making it more sensible to follow the patient up and keep the track of the right decisions. The patient is currently being followed, and we hope stability is getting to the point.
Conflict of Interest
The author declares no conflict of interest.
References
- Avila MP. Subretinal neovascularization: contribution on angiographic and therapeutic study of patients with age-related macular degeneration [dissertation]. Belo Horizonte Universidade Federal de Minas Gerais.1997.
- Bressler NM. Age-related macular degeneration is the leading cause of blindness. JAMA.2004;291:1900-1.
- Abrishami M, Zarei-Ghanavati S, Soroush D, et al. Preparation, characterization, and in vivo evaluation of nanoliposomes-encapsulated bevacizumab (avastin) for intravitreal administration Retina.2009;29: 699-703.
- Li LX, Turner JE. Transplantation of retinal pigment epithelial cells to immature and adult rat hosts short- and long-term survival.1988;47:77-85.
- Liu HA, Liu YL, Ma ZZ, et al. A lipid nanoparticle system improves RNA efficacy in RPE cells and a laser-induced murine CNV model. Invest Ophthalmol Vis Sci.2011;52:4789-94.
- Eye tech Study Group Preclinical and phase 1A clinical evaluation of an anti-VEGF pegylated aptamer (EYE001) for the treatment of exudative age-related macular degeneration. Retina.2002;22:143-52.
- Marano RJ, Toth I, Wimmer N, et al. Dendrimer delivery of an anti-VEGF oligonucleotide into the eye a long-term study into inhibition of laser-induced CNV, distribution, uptake and toxicity. Gene Ther.2005;12:1544-50.
- Marano RJ, Wimmer N, Kearns PS, et al. Inhibition of in vitro VEGF expression and choroidal neovascularization by synthetic dendrimer peptide mediated delivery of a sense oligonucleotide. Exp Eye Res.2004;79:525-35.
- Amico DJ, Goldberg MF, Hudson H, et al. Anecortave acetate as mono therapy for the treatment of sub-foveal lesions in patients with exudative Age related Macular Degeneration (AMD): interim (month 6) analysis of clinical safety and efficacy. Retina.2003;23:14-23.
- Interferon alpha-2a is ineffective for patients with choroid neovascularization secondary to age related macular degeneration. Arch Ophthalmol.1997;115:865-72.
- Schmidt Erfurth U, Miller JW, Sickenberg M, et al. Photodynamic therapy of sub foveal choroidal neovascularization in a phase I/II trial study Preliminary results of multiple treatments. Invest Ophthalmol Vis.Sci.1997;38:17.
- Laser treatment in eyes with large drusen. Short term effects seen in a pilot randomized trial. Ophthalmology.1998;105:11-23.
- Zhang K, Hopkins JJ, Heier JS, et al. Ciliary neurotrophic factor delivered by encapsulated cell intraocular implants for treatment of geographic atrophy in age-related macular degeneration. Proc Natl Acad Sci .U S A.2011;108:6241-5.
- Machemer R, Sugita G, Tano Y. Treatment of intraocular proliferations with intra-vitreal steroids. Trans Am Ophthalmol Soc.1979;77:171-80.
- Machemer R. Five cases in which a depot steroid (hydrocortisone acetate and methylprednisolone acetate) was injected into the eye. Retina.1996;16:166-7.
- Reilly MS, Boehm T, Shing Y, et al. Endostatin An endogenous inhibitor of angiogenesis and tumor growth. Cell.1997;88:277-85.
- Penfold PL, Wong JG, Gyory J. Effects of triamcinolone actinide on microglial morphology and quantitative expression of MHC-II in exudative age related macular degeneration. Clin Experiment Ophthalmol.2001;29:188-92.
- Pepic I, Hafner A, Lovric J, et al. A nonionic surfactant/chitosan micelle system in an innovative eye drop formulation, J Pharm Sci.2010;99:4317-25.
- Sieving PA, Caruso RC, Tao W, et al. Ciliary neurotrophic factor (CNTF) for human retinal degeneration: phase I trial of CNTF delivered by encapsulated cell intraocular implants. Proc Natl Acad Sci U S A. 2006;103:3896-3901.
- van Zeeburg EJ, Maaijwee KJ, Missotten TO, et al. A free retinal pigment epithelium-choroid graft in patients with exudative age- related macular degeneration results up to 7 years, Am J Ophthalmol.2012;153:120-7.
- Rosenfeld PJ, Schwartz SD, Blumenkranz MS, et al. Maximum tolerated dose of a humanized anti-vascular endothelial growth factor antibody fragment for treating neo-vascular age- related macular degeneration. Ophthalmology.2005;112:1048-53.
- Penfold PL, Madigan MC, Gillies MC, et al. Immunological and aetiological aspects of macular degeneration. Prog Retin Eye Res.2001;20:385-414.
- Barouch FC, Miller JW. Anti-vascular endothelial growth factor strategies for the treatment of choroidal neovascularization from age related macular degeneration. Int Ophthalmol Clin.2004;44: 23-32.
- Folkman J, Ingber DE. Angiostatic steroids. Method of discovery and mechanism of action. Ann Surg.1987;206:374-83.
- Haritoglou C, Tadayoni R, May CA, et al. Short-term in vivo evaluation of novel vital dyes for intraocular surgery. Retina.2006;26:673-8.
- Joussen AM, Kirchhof B. Angiogenesis in ophthalmology. A theme with a future. Ophthalmologe.2003;100:281-3.
- Michels S, Rosenfeld PJ. Treatment of neovascular agerelated macular degeneration with Ranibizumab Lucentis. Klin Monatsbl Augenheilkd.2005;222:480-4.
- Tolentino MJ, Brucker AJ, Fosnot J, et al. Intravitreal injection of vascular endothelial growth factor small interfering RNA inhibits growth and leakage in a nonhuman primate, laser induced model of choroidal neovascularization. Retina.2004;24:132-8.
- Van Wijngaarden P, Coster DJ, Williams KA. Inhibitors of ocular neovascularization: promises and potential problems JAMA.2005; 293:1509-13.
- Moshfeghi AA, Puliafito CA. Pegaptanib sodium for the treatment of neovascular age-related macular degeneration. Expert Opin Investig Drugs.2005;14:671-82.
- Iluvien 190 Micrograms Intra-vitreal Implant in Applicator, Public Assessment Report, Medicines and Healthcare products Regulatory Agency 2012.
- Kato A, Kimura H, Okabe K, et al. Suppression of laser-induced choroidal neovascularization by posterior sub tenon administration of triamcinolone acetonide.Retina.2005;25:503-9.
- Kameda T, Tsujikawa A, Otani A, et al. Polypoidal choroidal vasculopathy examined with en face optical coherence tomography. Clin Experiment Ophthalmol.2007;35:596-601.
- Honda S, Matsumiya W, Negi A. Polypoidal choroidal vasculopathy clinical features and genetic predisposition. Ophthalmologica.2014;231:59-74.
- Tan CS, Ngo WK, Chen JP, et al Everest study group. Everest study report 2 imaging and grading protocol, and baseline characteristics of a randomised controlled trial of polypoidal choroidal vasculopathy. Br J Ophthalmol.2015;99:624-8.
- Koizumi H, Yamagishi T, Yamazaki T, et al. Sub-foveal choroidal thickness in typical age related macular degeneration and polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol. 2011;249:1123-8.
- Cho HJ, Baek JS, Lee DW, et al. Short-term effectiveness of intravitreal bevacizumab vs. ranibizumab injections for patients with polypoidal choroidal vasculopathy. Korean J Ophthalmol.2012; 26:157-62.
- Pereira FB, Veloso CE, Kokame GT, et al. Characteristics of neovascular age-related macular degeneration in Brazilian patients. Ophthalmologica.2015;234:233-42.