Research Article - Biomedical Research (2017) Volume 28, Issue 8
The evaluation of deaths due to methyl alcohol intoxication
Omer Kurtas1, Kemal Yavuz Imre2, Erdal Ozer3*, Muhammet Can4, Ismail Birincioglu4, Celal Butun5,Guven Seckin Kirci3, Ali Yildirim5, Samet Kiyak6 and Riza Yilmaz6
1Department of Forensic Medicine, Kocaeli University, Faculty of Medicine, Kocaeli, Turkey
Department of Forensic Medicine, Omer Halis Demir University Research and Training Hospital, Ni?de, Turkey
3Department of Forensic Medicine, Karadeniz Technical University, Faculty of Medicine, Trabzon, Turkey
4Department of Forensic Medicine, Balikesir University, Faculty of Medicine, Balikesir, Turkey
5Department of Forensic Medicine, Cumhuriyet University, Faculty of Medicine, Sivas, Turkey
6Department of Forensic Medicine, Bulent Ecevit University, Faculty of Medicine, Zonguldak, Turkey
- *Corresponding Author:
- Erdal Ozer
Department of Forensic Medicine
Karadeniz Technical University, Trabzon, Turkey
Accepted on January 12, 2017
Abstract
Background: Methanol poisoning is a serious medical, social and economic problem that may cause severe illness or death. After methanol ingestion, central nervous system depression, headache, dizziness, nausea, lack of coordination, and confusion begins. Once the initial symptoms have passed, a second set of symptoms arises, 10 to 30 hours after the initial exposure to methanol, including blurring or complete loss of vision and acidosis. Methanol poisoning by ingestion is a world-wide problem, and in some regions it is connected with high morbidity and mortality. The lethal dose of methanol in humans shows pronounced individual differences ranging from 15 to 500 ml.
Methods: The records of the First Specialization Board of the Council of Forensic Medicine between 2002 and 2010 were reviewed retrospectively for all methyl alcohol poisoning cases.
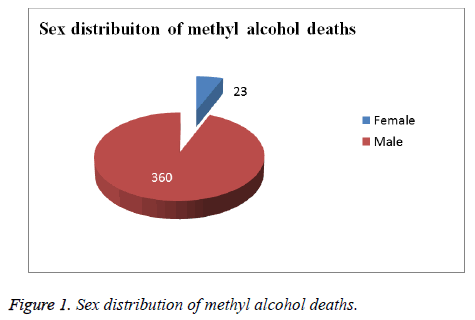
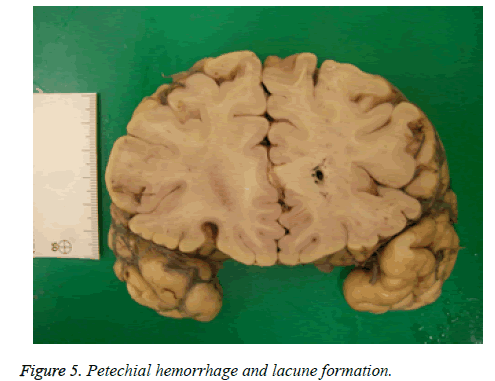
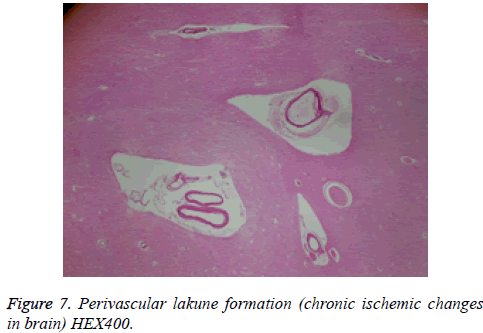
Results: There were 383 cases recorded. 360 (94%) of total fatalities were men and 23 (6%) were women. The age range was between 17 and 89. Although patients were conscious, cooperative, oriented at first, deteriorated general health state, metabolic acidosis and neurologic sequelae with severe electrocardiographic (ECG) changes were seen in progress of time. The laboratory findings and MRI imaging method were applied to assess progress and medical treatment. Unfortunately severe acidosis, central nervous system (CNS) sequelae and a lethal outcome occurred. The methyl alcohol blood concentrations ranged from 0 to 826 mg per 100 ml. The most common macroscopic and microscopic finding was lung edema, cerebral and cerebellar hemorrhage, ischemic changes in the brain and optic neuritis. Putaminal necrosis and hemorrhage, brainstem petechial hemorrhage, myocardial acute ischemic changes, thalamic and hypothalamic hemorrhage were detected rarely.
Conclusions: This is the first study to report postmortem findings, clinical reports, crime scene reports and eye witness accounts to investigate methyl alcohol poisoning cases from medico-legal point of view in Turkey. Methanol poisoning by ingestion is a world-wide problem with high morbidity and mortality. For preventing methanol deaths, both awareness and public education must be increased.
Keywords
Methanol, Poisoning, Forensic medicine.
Introduction
Methanol, known as methyl alcohol or wood alcohol, is a chemical with the formula CH3OH. Methanol is a light, volatile, colourless, flammable liquid with a distinctive odor very similar to, but slightly sweeter than, that of ethanol and produced as a by-product of the distillation of wood. It is used as antifreeze, solvent, fuel, and denaturant for ethanol. Methanol ingestion is an uncommon form of poisoning that can cause severe metabolic disturbances, blindness, permanent neurologic dysfunction and death. On the other hand methanol itself may be harmless; it is converted to the highly toxic formic acid in the human body. Methanol poisoning is a serious medical, social and economic problem may cause severe illness or death [1-4].
Accidental, mass killing, suicidal, methanol poisonings can occur both in developed and developing countries [5-7]. Most of acute methanol toxicity cases result from accidental ingestion [8]. Methanol itself is not highly toxic, but it is metabolised to toxic metabolites like formaldehyde and formic acid which cause metabolic acidosis, blindness, cardiovascular instability, and death [2,9-11]. Minimal lethal dose of methanol in humans has been assumed to be 1 gram per kg of body weight [12]. Methanol is fatal due to CNS depressant properties and effects of metabolites [13], and converted to formaldehyde formaldehyde is converted to formic acid [14]. Formic acid inhibits mitochondrial cytochrome c oxidase, causing the symptoms of hypoxia at the cellular level, and also causing metabolic acidosis [15].
After methanol ingestion, central nervous system depression, headache, dizziness, nausea, lack of coordination, and confusion begins. Once the initial symptoms have passed, a second set of symptoms arises, 10 to 30 hours after the initial exposure to methanol, including blurring or complete loss of vision and acidosis [13]. These symptoms result from the accumulation of toxic levels of formic acid in the blood, and may progress to death by respiratory failure. MRI findings in methanol poisoning are characteristic and include hemorrhagic putaminal necrosis, subcortical and deep white matter lesions, cerebral and cerebellar cortical lesions, and midbrain lesions [16-19].
Methanol poisoning by ingestion is a world-wide problem, and in some regions it is connected with high morbidity and mortality. The lethal dose of methanol in humans shows pronounced individual differences ranging from 15 to 500 ml.
In our study, our aim was to investigate methyl alcohol poisoning cases from medico-legal point of view in Turkey.
Materials and Methods
The Council of Forensic Medicine is an official organ of the Ministry of Justice and the only official expert in forensic medicine in Turkey. The duties and responsibilities of the Council of Forensic Medicine are determined by the law. Each year approximately 85,000 reports about scientific and technical subjects related to forensic sciences requested by the courts and the district attorneys are written by the council. The Council of Forensic Medicine includes specialized departments such as morgue and toxicology departments and branches such as the first branch which deals with autopsy, toxicological analyses and medical and legal records.
Details of autopsies performed in the cities of Turkey since 2001 have been recorded in a database in the first branch which deals with the cause of death. The first branch includes a general surgeon, a cardiovascular surgeon, a neurosurgeon, a gynecologist, an internist, a cardiologist, a hematologist, an immunologist, a pathologist and a forensic specialist. The study included the cases in which the cause of death was documented as methyl alcohol intoxication in the reports from the first branch of the Council of Forensic Medicine. The records of the First Specialization branch of the Council of Forensic Medicine between 2002 and 2010 were reviewed retrospectively for all methyl alcohol poisoning cases. All the records had witness statements, crime scene reports, medical reports and autopsy reports with histopathological and toxicological reports. 398 death cases were identified and were reportedly linked to ingestion of methyl alcohol poisoning. Because of only available witness statements, we excluded 15 cases without any relevant toxicological evidence, medical reports or necroptic examinations. The remaining 383 cases were evaluated based on age, gender, hospital records if present, macroscopic, microscopic, methyl alcohol blood levels and other chemical evidence gathered during autopsy with witness statements.
Results
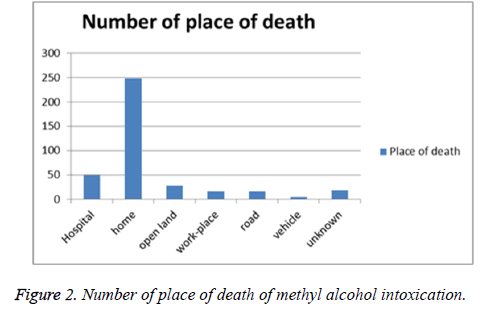
There were 383 deaths due to methanol poisoning between the years of 2002 and 2010. 360 (94%) of total fatalities were men and 23 (6%) were women (Figure 1). The age range was between 17 and 89. Regarding the distribution of the places of death, it was observed that 49 cases (12.8 %) died in a hospital, as well as 248 cases (64.7%) found dead at home, 29 cases (7.5%) found dead at open land, 17 cases (4.4%) found workplace, 16 cases (4.2%) found dead on the road, 5 cases (1.3%) found in a vehicle and the resting are not known where they died (Figure 2).
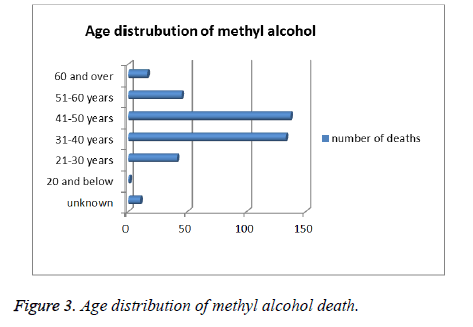
There was 1 case aged 20 years and below, 41 cases between 21-30 years, 133 cases between 31-40 years, 137 cases between 41-50 years, 45 cases between 51-60 years and 16 cases aged 60 years and above (Figure 3). The age of 10 cases were unknown. The methyl alcohol blood concentrations ranged from 0 to 826 mg per 100 ml.
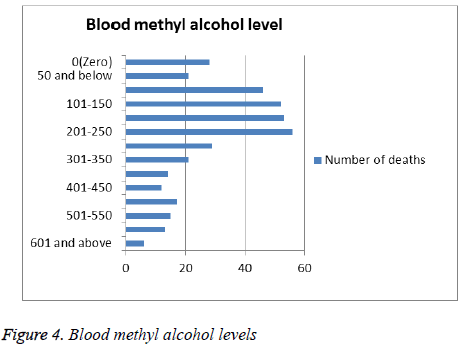
21 of 49 cases admitted to hospital died within several hours, and blood methyl alcohol levels obtained in the autopsies of these 21 people have been below the level 50 mg per 100 ml. The remaining 28 people died within 4-13 days of hospital treatment, but blood methanol levels were not measured during hospital stay. Despite the autopsy blood methyl alcohol levels of these cases were zero, it was decided that death had occurred duo to toxicity from methyl alcohol according to macroscopic and microscopic autopsy findings, clinical findings and witness statements. Blood methyl alcohol levels of other 334 cases were above 100 mg per 100 ml (Figure 4).
28 of 49 patients admitted to hospitals with complaints of blurred vision, nausea, and inability to maintain balance. At first, they were conscious, cooperative, oriented. Vital signs (blood pressure (BP), pulse (P), respiratory rate (RR) were detected at normal levels. Neurological examination of the patients was natural but at ophtalmologic examinations the most important findings were hyperaemia on the optic discs. With the diagnosis of methanol poisoning, they were taken into emergency department observation unit and treatment process was started. The following laboratory values were gained: arterial blood gases: pH, PCO2, PO2, HCO3, Glucose, BUN, creatinine in Table 1. Ethyl alcohol treatments and dialysis were administered to most patients. Glasgow Coma Scales (GCS) were deteriorated over time. Then the physical examinations revealed a moderately or severely deteriorated general health state, metabolic acidosis and neurologic sequelae. The Drug and Poison Information Center was consulted for potential development of complications, and information about treatment alternatives was obtained. This Center indicated first clinical signs of visual toxicity, indicating hemodialysis, severe electrocardiographic (ECG) changes, with sinus tachycardia, PR prolongation, QTc prolongation, and non-specific T-wave changes, severe acidosis, central nervous system (CNS) sequelae and a lethal outcome. The hospital stay after onset of methanol poisoning ranged from 4 to 13 days. Demographics and poorest clinical laboratory findings of metil alcohol ingestion cases treated in hospitals are showed in Table 1. Within the period of hospital stay some patients were applied MRI imaging method. Pathological findings were found in 9 patients examined by MRI imaging method. These lesions were in the putamen-2 cases, haemorrhage-2 cases, deposits in white matter-1 case, globus pallidus-1 case, brainstem-1 case and multipl lesions -2 cases. Macroscopic and microscopic autopsy findings shown in Table 2 and Figures 5-7 were not directly associated with methyl alcohol intoxication.
| Case Number | Age | Sex | pH | pCO2 | pO2 | HCO3 | BUN mg/dL | Creatinine mg/dL | Glucose mg/dL |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 22 | M | 6.4 | 31.2 | 46 | 12.6 | 48 | 10.1 | 198 |
| 2 | 37 | M | 7.16 | 14.6 | 58 | 9.5 | 54 | 11.3 | 149 |
| 3 | 34 | M | 7.19 | 32.5 | 42 | 16.2 | 51 | 14.2 | 198 |
| 4 | 39 | M | 6.35 | 21 | 24 | 11.6 | 58 | 16.2 | 149 |
| 5 | 48 | M | 7.16 | 13.6 | 48 | 9.9 | 44 | 21.1 | 306 |
| 6 | 35 | F | 6.33 | 16.6 | 77 | 12.1 | 41 | 18.3 | 288.78 |
| 7 | 33 | F | 7.16 | 32.9 | 62 | 9.4 | 49 | 10.2 | 188 |
| 8 | 42 | M | 6.39 | 22.3 | 76 | 15.2 | 52 | 15.1 | 145 |
| 9 | 28 | M | 6.4 | 16.5 | 52 | 10.9 | 57 | 17.3 | 306.7 |
| 10 | 37 | M | 7.19 | 17.6 | 70 | 17.2 | 48 | 10.8 | 198 |
| 11 | 44 | M | 7.01 | 33.5 | 54 | 15.9 | 54 | 16.9 | 149 |
| 12 | 49 | M | 6.972 | 29.4 | 63.4 | 9.6 | 49 | 11.6 | 306 |
| 13 | 42 | M | 7.161 | 30.5 | 48.7 | 10.2 | 59 | 14.4 | 129 |
| 14 | 29 | M | 7.01 | 28 | 64 | 12.9 | 39 | 14.1 | 176 |
| 15 | 32 | M | 7.059 | 16.2 | 42.6 | 14.1 | 42 | 21.3 | 195 |
| 16 | 41 | F | 7.11 | 14.3 | 41 | 12.8 | 57 | 23.2 | 165 |
| 17 | 28 | M | 7.21 | 20.3 | 74 | 9 | 47 | 17.6 | 198 |
| 18 | 58 | M | 7.05 | 32.2 | 69.5 | 15.2 | 43 | 18.9 | 149 |
| 19 | 89 | F | 7.29 | 27.8 | 59 | 17.1 | 55 | 19.2 | 306 |
| 20 | 42 | M | 7.16 | 16.9 | 64 | 13.6 | 58 | 20.1 | 145 |
| 21 | 26 | M | 7.15 | 30.2 | 75.5 | 9.1 | 43 | 19.7 | 195 |
| 22 | 50 | M | 7.005 | 21.9 | 69.5 | 17.7 | 49 | 15.5 | 169 |
| 23 | 77 | M | 7.09 | 22.8 | 47 | 10.2 | 58 | 19.1 | 129 |
| 24 | 32 | F | 7.161 | 31.8 | 59 | 10.1 | 57 | 10.7 | 198 |
| 25 | 41 | M | 7.011 | 21.7 | 52 | 9.7 | 44 | 22.8 | 149 |
| 26 | 28 | M | 7.1 | 30.5 | 70 | 11.4 | 56 | 19.1 | 306 |
| 27 | 58 | M | 7.06 | 21.3 | 57 | 9.8 | 52 | 17.3 | 145 |
| 28 | 32 | M | 7.09 | 29.6 | 61 | 19.2 | 47 | 24.7 | 195 |
pCO2: Carbon dioxide Partial Pressure; pO2: Oxygen Partial Pressure; HCO3: Carbonate; BUN: Blood Urea Nitrogen
Table 1. Demographics, and poorest clinical laboratory findings of metil alcohol ingestion cases treated in hospitals.
| Autopsy Findings | Macroscopic (number of cases) | Microscopic (number of cases) | |
|---|---|---|---|
| Brain | Cortical ischemia | 3 | 12 |
| Cerebral and cerebellar hemorrhage | 19 | 19 | |
| Putaminal necrosis and hemorrhage | 4 | 7 | |
| Thalamic and hypothalamic hemorrhage | 1 | 3 | |
| brainstem petechial hemorrhage | 3 | 5 | |
| Optic neuritis | 0 | 9 | |
| Hyperemia | 122 | 98 | |
| Cerebral edema | 15 | 11 | |
| Autolysis | 7 | 7 | |
| Postmortem changes | 87 | 51 | |
| Hearth | Myocardial acute ischemic changes | 0 | 4 |
| Hyperemia | 87 | 77 | |
| Hypertrophy | 23 | 23 | |
| Fibrous scarring | 8 | 8 | |
| Autolysis | 7 | 7 | |
| Postmortem changes | 118 | 97 | |
| Lung | Lung edema-congestion | 33 | 16 |
| Hyperemia | 62 | 41 | |
| Intra-alveolar hemorrhage | 4 | 4 | |
| Subplevral hemorrhage | 9 | 0 | |
| Bronchiectasis | 3 | 3 | |
| Chronic bronchitis | 3 | 3 | |
| Pneumonia | 15 | 15 | |
| Autolysis | 7 | 7 | |
| Postmortem changes | 115 | 77 | |
| Liver | Hyperemia | 48 | 36 |
| Fatty change in liver | 43 | 41 | |
| Autolysis | 5 | 5 | |
| Postmortem changes | 112 | 83 | |
| Kidney | Hyperemia | 76 | 51 |
| Parenchymal degeneration | 3 | 3 | |
| Tubular injury | 2 | 28 | |
| Tubular necrosis | 3 | 21 | |
| Retantion cyst | 16 | 0 | |
| Autolysis | 5 | 5 | |
| Postmortem changes | 96 | 73 |
Table 2. Macroscopic and microscopic autopsy findings.
Discussion
This is the first study to report postmortem findings, clinical reports, crime scene reports and eye witness accounts in Turkey in an unselected series of fatal methyl alcohol intoxication. This study did not show the frequency of methyl alcohol intoxication deaths at both medical records and autopsies in Turkey. Because the courts and the district attorneys ask the Council of Forensic Medicine how death happens only when there is a suspicious situation, all methyl alcohol intoxication deaths are not sent to the Council of Forensic Medicine. Three hundred and eighty three cases reported here were representative of deaths thought to be caused by methyl alcohol intoxication.
Sporadic or epidemic accidental use of methyl alcohol is one of the basic problems that forensic medicine professionals have to face in the whole world. Alcoholics know that ethanol may have harmful effects they intentionally substituted methanolcontaining substances. In addition to sporadic cases several large epidemics have been reported [20-23]. When we look at the list of methanol poisoning outbreaks in the world, we see the outbreaks in 14 countries including Turkey. Most events have come into existence in India from 1976 to 2015 and died more than 1900 people [24]. Three major methanol outbreaks in Libya (2013) and Kenya (May and July 2014) occurred [25]. Four outbreaks were registered from Turkey and they were 21 deaths in 2004, 23 deaths in 2005, 5 deaths in 2011 and 32 deaths in 2015 [24]. Because our database about methyl alcohol poisoning was between 2002 and 2010, it includes most cases of the two outbreaks from 21 deaths in 2004 and 23 deaths in 2005. In November 30, 2015 the number of people died from bootleg alcohol poisoning or counterfeit raki in the city of Izmir rose to eight. In October 08, 2015, 4 cases died in the city of Mersin, In October 18, 2015, a total of 89 cases, including 12 people were died in the city of Istanbul, in March 22, 2009, 4 cases died in the city of Bursa in Turkey [26-29].
In our study, 360 (94%) of total fatalities were men and 23 (6%) were women. There is male dominance in our study. Male dominance also is seen in other studies. Azmak et al. claimed that male dominance can be explained by the habitual consumption of alcohol especially, methanol by males more than females [30]. We also think that males have habitual consumption of methanol more than females. In our study, the largest age group was 41-50 years old with 137 cases, followed by 31-40 years with 133 cases. 45 of the cases were between 51-60 years, 41 of the cases were between 21-30 years old, 16 of the cases were 60 and above and only 1 of the cases was under 20 years old. In 10 cases age of the deceased could not be determined. Azmak et al. in his study found that deaths mostly occurred between 41 and 45 years of age 30, thus showing similar results as reported in previous studies [31-34]. Findings indicate that methanol fatalities are important causes of middle age mortalities, which are currently at the highest point [30]. Our largest group was 41-50 years old with 137 cases which are similar to Azmak et al’s findings.
Liu et al., Inanici et al. and Meyer et al. stated that, individuals had an asymptomatic period of approximately 12-24 hours, following consumption of the alcoholic beverage [33-35]. Yayc? et al. in their 8 years study indicated that the cases continued to consume the alcoholic beverage until they recognized the intoxication symptoms, at which point it is too late for admission to hospital. This can explain the 77.5% fatality rate [31]. We found, time of remaining alive after methanol ingestion as 0 to 30 minutes in 39% (149 cases), 1 to 24 hours in 21% (81 cases) cases, 1to 12 days in 64 cases, 13 days and above in 8 cases. Remaining alive time after methanol ingestion was unknown in 81 of the cases. Although ocular morbidity caused by methanol poisoning is well known, the lethal dose of the methyl alcohol for humans is not known for certain, but evidence suggests that it can vary over a wide range. The minimum lethal dose is often cited as about 100 ml, but Bennett et al. [36] reported a fatal poisoning following ingestion of only 15 ml of 40% methanol and Ziegler [37] reported a fatal case involving one ounce. On the other hand, ingestions of more than 500 ml have reportedly occurred without causing death or blindness [38]. According to Maio et al. and Maio [39], the minimum lethal blood level in methanol poisoning is approximately 80 mg per 100 ml. Yayci et al., Elmas et al., Davis et al., Inacici et al. stated that the blood methanol concentrations, in their studies, ranged widely from 55 to 479 mg per 100 ml. There were 17 (94.4%) cases with the blood methanol level over 80 mg per 100 ml similar to other studies [30-32,34,40]. In our study the methyl alcohol blood concentrations ranged widely from 0 to 826/100 ml. There were 288 cases (75.2%) with the methyl alcohol blood concentrations over 100 mg/dl. These values are higher than the values reported as 80-100 mg/dl which is a range of the lethal dose [3,41]. In another study, in 15 fatalities following hospital admission for methanol intoxication, postmortem heart blood methanol concentrations ranged from 23 to 268 mg/dl [42]. In the studies of Derrick et al. [42] and Mittal et al. [43], showed that the lethal dose of methanol in humans showed pronounced individual differences, ranging from 15 to 500 mg⁄dL. Karadeniz et al. and Birincioglu et al. in their study, found that the blood methanol concentration also ranged widely, from 15 to 482 mg/dL. They had eight cases (61.5%) with methyl alcohol blood concentration over 100 mg/dL, and five cases below 50 mg/dL [44]. Other studies of methyl alcohol concentrations have reported varying ranges as follows: 55-479 mg⁄dL by Azmak et al. [30], 50-755 mg/dL by Yayci et al. [31], 38-414 mg/dL by Fedakar et al. [45], and 350-450 mg/dL by Andersen et al. [46].
Paliwal et al. [47] suggested that haemorrhagic putaminal necrosis, optic atrophy and coma were a triad of methanol poisoning. Vaneckova et al. [48] showed that almost half of the patients who survived acute methanol poisoning had pathological findings by MRI. When we searched the medical records there were 2 cases with haemorrhagic putaminal necrosis, optic atrophy and coma. Haemorrhagic putaminal necrosis was confirmed in the 2 patients who had long-term treatments by MRI imaging method. In 28 of the 49 cases treated in the hospital, blood methyl alcohol concentration was measured during the autopsy for it was not however examined at first application or during the hospital stay period. The measured blood methanol concentration was zero. In other cases treated in the hospital, 21 had blood concentrations lower than 50 mg per 100 ml, while 334 cases had blood levels higher than 50 mg per 100 ml (Figure 4). The nervous system and specifically the visual system have increased susceptibility for methanol intoxication. Specific histopathological lesions in central nervous system were identified in relation with life span of cases after methyl alcohol ingestion. Patients surviving methanol intoxications have been observed to develop cystic necrosis of the putamen, laminar necrosis of the cerebral cortex and cystic necrosis of cerebral white matter. In this study 19 cerebral and cerebellar hemorrhage, 12 cortical ischemia, 7 putaminal necrosis and hemorrhage, 3 thalamic and hypothalamic hemorrhage, 5 brainstem petechial hemorrhage, 7 optic neuritis were observed (Table 2). Many topographic sampling should be carried out primarily central nervous system and the other organs of cases susceptible to methyl alcohol poisoning.
In Turkey, which is an undeveloped Middle East Country, the high tax on the alcoholic beverages, called special consumption tax, was established first in 2002 and dramatically increased in 2010 by the government led to a significant rise of smuggling and fraud involving the alcoholic beverages in the country. Bootlegging is blamed for the 2011 Turkish Riviera mass alcohol poisoning, in which five innocent Russian tourists died [49]. Prevention of the illegal production of methanol and methylated spirits’ should be established. For preventing methanol deaths, awareness in the whole country must be increased. Harms of methanol, the products that contain methanol must be a routine public education. Media, especially television can be used for this. Doctors must be educated about methanol poisoning; so that they can be aware of the symptoms and know how to treat the patients.
References
- Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2014 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicol 2015; 53: 962-1147.
- Jacobsen D, McMartin KE. Antidotes for methanol and ethylene glycol poisoning. J Toxicol Clin Toxicol 1997; 35: 127-143.
- Kruse JA. Methanol poisoning. Intensive Care Med 1992; 18: 391-397.
- Institute for Occupational Safety and Health. "The Emergency Response Safety and Health Database: Methanol". 2009.
- Paasma R, Hovda KE, Jacobsen D. Methanol Poisoning and Long Term Sequelae-a Six Years Follow-up after a Large Methanol Outbreak. BMC Clin Pharm 2009; 9: 5.
- Epker JL, Bakker J. Accidental methanol ingestion: case report. BMC Emerg Med 2010; 10: 3.
- Bucaretchi F, De Capitani EM, Madureira PR, Cesconetto DM, Lanaro R. Suicide attempt using pure methanol with hospitalization of the patient soon after ingestion: case report. Sao Paulo Med J 2009; 127: 108-110.
- Xiao JH. Accidental methyl alcohol poisoning. Zhonghua Yu Fang Yi Xue Za Zhi 1990; 24: 160-162.
- Martin-Amat G, McMartin KE, Hayreh SS, Hayreh MS, Tephly TR. Methanol poisoning: ocular toxicity produced by formate. Toxicol Appl Pharmacol 1978; 45: 201-208.
- Sejersted OM, Jacobsen D, Ovrebø S, Jansen H. Formate concentrations in plasma from patients poisoned with methanol. Acta Med Scand 1983; 213: 105-110.
- Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA. American Academy of Clinical Toxicology Ad Hoc Committee on the Treatment Guidelines for Methanol Poisoning. American Academy of Clinical Toxicology Practice Guidelines on the Treatment of Methanol Poisoning Journal of Toxicology. Clin Toxicol 2002; 40: 415-446.
- Röe O. Species differences in methanol poisoning. Crit Rev Toxicol 1982; 10: 275-286.
- Schep LJ, Slaughter RJ, Vale JA, Beasley DM. A seaman with blindness and confusion. BMJ 2009; 339: b3929.
- McMartin KE, Martin-Amat G, Noker PE, Tephly TR. Lack of a role for formaldehyde in methanol poisoning in the monkey. Biochem Pharmacol 1979; 28: 645-649.
- Liesivuori J, Savolainen H. Methanol and formic acid toxicity: biochemical mechanisms. Pharmacol Toxicol 1991; 69: 157-163.
- Halavaara J, Valanne L, Setälä K. Neuroimaging supports the clinical diagnosis of methanol poisoning. Neuroradiol 2002; 44: 924-928.
- Rubinstein D, Escott E, Kelly JP. Methanol intoxication with putaminal and white matter necrosis: MR and CT findings. AJNR Am J Neuroradiol 1995; 16: 1492-1494.
- Hsu HH, Chen CY, Chen FH, Lee CC, Chou TY. Optic atrophy and cerebral infarcts caused by methanol intoxication: MRI. Neuroradiol 1997; 39: 192-194.
- Sefidbakht S, Rasekhi AR, Kamali K, Borhani Haghighi A, Salooti A. Methanol poisoning: acute MR and CT findings in nine patients. Neuroradiol 2007; 49: 427-435.
- Naraqi S, Dethlefs RF, Slobodniuk RA, Sairere JS. An outbreak of acute methyl alcohol intoxication. Aust N Z J Med 1979; 9: 65-68.
- Kane RL, Talbert W, Harlan J, Sizemore G, Cataland S. A methanol poisoning outbreak in Kentucky. A clinical epidemiologic study. Arch Environ Health 1968; 17: 119-129.
- Benton CD, Calhoun EP. The ocular effects of methyl alcohol poisoning; report of a catastrophe involving 320 persons. Am J Ophthalmol 1953; 36: 1677-1685.
- Swartz RD, Millman RP, Billi JE. Epidemic methanol poisoning: clinical and biochemical analysis of a recent episode. Medicine 1981; 60: 373-382.
- https://en.wikipedia.org/wiki/List_of_methanol_poisoning_incidents#Turkey
- Rostrup M, Edwards JK, Abukalish M, Ezzabi M, Some D, Ritter H, Menge T, Abdelrahman A, Rootwelt R, Janssens B, Lind K, Paasma R, Hovda KE. The Methanol Poisoning Outbreaks in Libya 2013 and Kenya 2014. PLoS One. 2016; 11:e0152676.
- http://www.hurriyetdailynews.com/bootleg-alcohol-death-toll-rises-to-eight-in-izmir.aspx?pageID=238&nID=91867&NewsCatID=509
- http://www.ntv.com.tr/turkiye/mersinde-4-olumde-sahte-icki-suphesi,Jw-bcr2JsEKIXuNzZf99Rw
- http://www.diken.com.tr/sahte-rakida-olenlerin-sayisi-23e-yukseldi-14-kisi-tutuklandi/
- http://www.sesgazetesi.com.tr/guncel/bursada-sahte-rakidan-olenlerin-sayisi-4-oldu/4925
- Azmak D. Methanol related deaths in Edirne. Leg Med 2006; 8: 39-42.
- Yayci N, A?ritmi? H, Turla A, Koç S. Fatalities due to methyl alcohol intoxication in Turkey: an 8-year study. Forensic Sci Int 2003; 131: 36-41.
- Elmas I, Tuzun B, Imrag C, Korkut M. Evaluation of deaths due to methyl alcohol intoxication with respect of forensic medicine. Istanbul Med Faculty 1996; 59: 64-69.
- Liu JJ, Daya MR, Mann NC. Methanol-related deaths in Ontario. J Toxicol Clin Toxicol 1999; 37: 69-73.
- Inanici MA, Birgen N, Anolay N. Methyl alcohol poisoning: an autopsy study. Proc 18th Congress Int Acad Legal Med, 2000; 36.
- Meyer RJ, Beard ME, Ardagh MW, Henderson S. Methanol poisoning. N Z Med J 2000; 113: 11-13.
- Bennett IL, Cary FH, Mitchell GL, Cooper MN. Acute methyl alcohol poisoning: a review based on experiences in an outbreak of 323 cases. Medicine 1953; 32: 431-463.
- Ziegler SL. The ocular menace of wood alcohol. Br J Opthalmol 1921; 5: 365-373.
- Tong TG. The alcohols. Crit Care Q 1982; 4: 75-85.
- Di Maio DJ, Di Maio VJM. Forensic pathology. (2ndedn). CRC Press, Boca Raton, 1993: 450-451.
- Davis LE, Hudson D, Benson BE, Jones Easom LA, Coleman JK. Methanol poisoning exposures in the United States: 1993-1998. J Toxicol Clin Toxicol 2002; 40: 499-505.
- Suit PF, Estes ML. Methanol intoxication: clinical features and differential diagnosis. Cleve Clin J Med, 1990. 57: pp 464-471.
- Derrick J, Pounder A, Jones W. Measuring alcohol postmortem. In: Karch SB, editor-in-chief. Drug abuse handbook. Washington, DC: CRC Press, 1998: 341–62.
- Mittal BV, Desai AP, Khade KR. Methyl alcohol poisoning: an autopsy study of 28 cases. J Postgrad Med 1991; 37: 9-13.
- Karadeniz H, Birincioglu I. Methyl alcohol poisoning in Trabzon (Turkey). J Forensic Sci 2011; 56: 822-824.
- Fedakar R, Turkmen N. Fatal poisonings in the south Marmara region of Turkey, 1996–2003. Eur J Gen Med 2008; 5: 1-8.
- Andersen H, Schmoldt H, Matschke J, Flachskampf FA, Turk EE. Fatal methanol intoxication with different survival times-Morphological findings and postmortem methanol distribution. Forensic Sci Int 2008; 179: 206-210.
- Paliwal VK, Uniyal R, Azim A, Neyaz Z, Muzaffar SN, Baronia AK. Haemorrhagic putaminal necrosis, optic atrophy and coma: a triad suggestive of methanol poisoning. Anaesth Crit Care Pain Med 2016; 44: 636-637.
- Vaneckova M, Zakharov S, Klempir J, Ruzicka E, Bezdicek O, Brozova H, Diblik P, Miovsky M, Hubacek JA, Urban P, Ridzon P, Pelclova D, Burgetova A, Masek M, Kotikova K, Peterova K, Liskova I, Hamplova L, Seidl Z. Neuro Endocrinol Lett. Imaging findings after methanol intoxication (cohort of 46 patients). 2015; 36: 737-744.
- Http://en.wikipedia.org/wiki/Alcohol_laws_of_Turkey